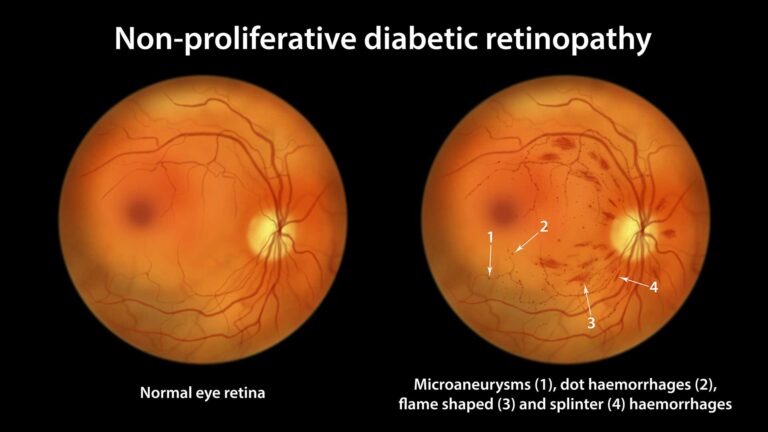
Rethinking NPDR: From a Single Pathway to Three Distinct Phenotypes
As vitreoretinal surgeons, we recognize that not all patients with nonproliferative diabetic retinopathy (NPDR) progress to vision-threatening complications. A groundbreaking review by Cunha-Vaz et al. (2025) reframes our understanding of NPDR progression by identifying three distinct disease phenotypes, each with different risks for developing clinically significant macular edema (CSMO) or proliferative diabetic retinopathy (PDR). This paradigm shift, enabled by modern non-invasive imaging, offers a more personalized approach to risk stratification and management.
🔍 The Three Phenotypes of Early Diabetic Retinal Disease
The authors propose that NPDR progression follows three primary pathways, which may occur alone or in combination:
-
Phenotype A: Neurodegeneration-Dominant
-
Hallmark: Progressive thinning of the ganglion cell layer + inner plexiform layer (GCL+IPL).
-
Imaging: OCT.
-
Progression: Slow. Eyes with this phenotype (approx. 50% of mild NPDR) showed no progression to CSMO or PDR in a 5-year study.
-
-
Phenotype B: Blood-Retinal Barrier (BRB) Breakdown-Dominant
-
Hallmark: Subclinical macular edema, increased vascular permeability.
-
Imaging: OCT for retinal thickness.
-
Progression: Intermediate risk. Combined with Phenotype A, these groups represent ~75% of mild NPDR with a low risk of vision-threatening complications.
-
-
Phenotype C: Ischemia-Dominant
-
Hallmark: Progressive capillary non-perfusion (hypoperfusion).
-
Imaging: OCT Angiography (OCTA) is key, showing decreased skeletonized vessel density (SVD) and perfusion density (PD).
-
Progression: High Risk. This is the only phenotype strongly associated with progression to CSMO and PDR.
-
Key Takeaway: Identifying the ischemic phenotype (C) is critical, as it signals the patient is on a high-risk trajectory.
📈 The Ischemic Phenotype: A Two-Stage Model
For high-risk Phenotype C eyes, progression follows a sequence:
-
Hypoperfusion Stage:
-
Characterized by progressive capillary closure.
-
Measured by decreasing SVD/PD on OCTA.
-
Closure begins in the superficial capillary plexus (SCP), then involves the deep capillary plexus (DCP), starting centrally and extending peripherally.
-
-
Hyperperfusion Stage:
-
A compensatory, dysregulated response to ischemia.
-
Characterized by the development of intraretinal microvascular abnormalities (IRMAs) and dilated shunt vessels.
-
Surrogate Marker: A rapid increase in microaneurysm (MA) count and turnover on color fundus photography (CFP).
-
This inflammatory, pro-angiogenic environment sets the stage for CSMO and PDR.
-
Clinical Implication: Monitoring the balance between hypoperfusion (OCTA metrics) and hyperperfusion (MA turnover) allows dynamic risk assessment.
🛠️ Practical Implications for the Vitreoretinal Surgeon
-
Incorporate OCTA into Routine Assessment: For patients with moderate NPDR (ETDRS 43+) or those progressing rapidly, OCTA is no longer just a research tool. It is essential for identifying the ischemic phenotype by quantifying capillary dropout.
-
Risk Stratify by Phenotype, Not Just ETDRS Level: A patient with moderate NPDR (ETDRS 43) and significant capillary non-perfusion on OCTA (Phenotype C) is at far greater risk than a patient with the same ETDRS level but a neurodegeneration-dominant profile (Phenotype A).
-
Monitor Progression with Combined Imaging:
-
OCTA tracks the hypoperfusion stage (SVD/PD decline).
-
CFP tracks the hyperperfusion response (rising MA turnover).
-
Together, they signal acceleration toward vision-threatening complications.
-
-
Tailor Management and Follow-up: Patients identified as Phenotype C warrant more frequent monitoring and earlier consideration of systemic or local interventions to halt ischemic progression.
Understanding NPDR Progression: Phenotypes & Imaging
This quiz tests your understanding of the three-pathway model of Nonproliferative Diabetic Retinopathy (NPDR) progression, as detailed in the recent review by Cunha-Vaz et al. (2025). Focus on the role of non-invasive imaging (OCT, OCTA) in identifying high-risk phenotypes.
1. According to the review, which of the three proposed NPDR phenotypes is exclusively associated with progression to vision-threatening complications (CSMO/PDR)?
Longitudinal studies show that only eyes with the ischemic phenotype (characterized by progressive capillary non-perfusion) progress to CSMO and PDR. Phenotypes A and B (neurodegeneration and BRB breakdown) have a much lower risk.
2. What is the primary non-invasive imaging modality recommended for identifying and quantifying the “Hypoperfusion Stage” of the ischemic phenotype (Phenotype C)?
OCTA provides direct, non-invasive visualization of the retinal capillary networks. It allows quantification of capillary dropout through metrics like Skeletonized Vessel Density (SVD) and Perfusion Density (PD), which are essential for identifying the progressive hypoperfusion that defines the high-risk phenotype.
3. In the two-stage model of ischemic phenotype progression, what is the best surrogate marker on clinical imaging for the “Hyperperfusion Stage” and the development of IRMAs?
The hyperperfusion response is characterized by the formation of dilated shunt vessels and IRMAs. Studies show a strong correlation between a rapid increase in MA number/formation rate and the development of these abnormal vessels, making MA turnover a practical clinical surrogate.
4. Which of the following best describes the typical spatial progression of capillary non-perfusion (hypoperfusion) in the ischemic phenotype?
OCTA studies demonstrate that capillary closure is first detected in the SCP. As the ischemia progresses, the DCP becomes involved. This progression is also characterized by a spread from the central macula outward to the periphery.
5. What is the major clinical implication of identifying a patient’s NPDR as primarily “Phenotype A” (Neurodegeneration-dominant)?
Eyes with Phenotype A (and B) represented about 75% of a mild NPDR cohort in a 5-year study and did not progress to CSMO or PDR. This phenotype identification allows for risk stratification and may permit less aggressive monitoring compared to the high-risk ischemic Phenotype C.
Quiz Complete
Your Score: 0/5
My score 5/5
It was interesting to me that all NPDR isnt created equal.
Combined imaging approach:
OCTA → hypoperfusion tracking.
CFP → hyperperfusion monitoring.
Tailored management:
Phenotype C patients need closer follow-up and earlier interventions.
👌💐
Phenotype C: Ischemia-Dominant
High Risk for progression to CSMO
and PDR
Thanks.🌺.. OCTA can be used for early detection of this phenotype.