Posted inInteresting Papers
Visual Loss in Geographic Atrophy
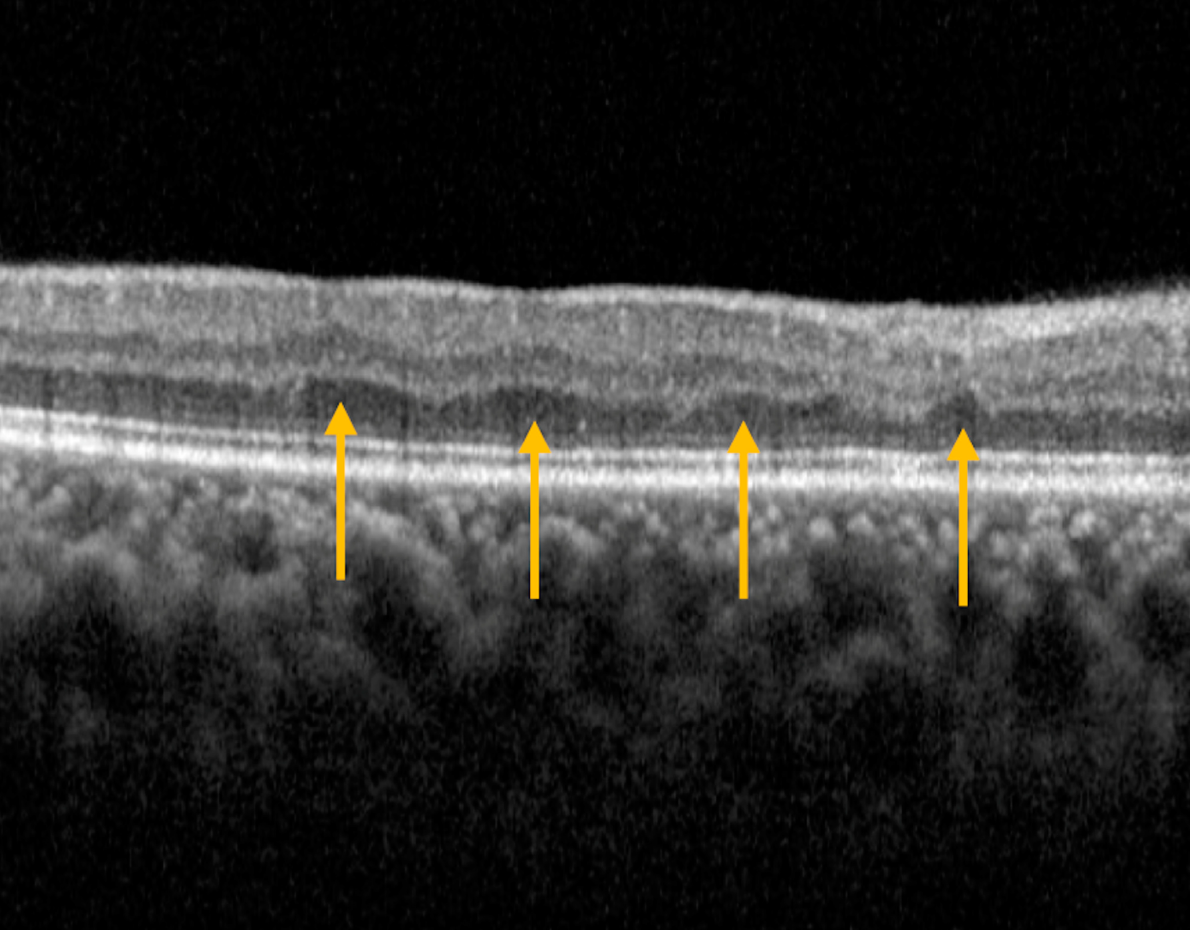
This study examines factors influencing visual loss in geographic atrophy (GA) related to age-related macular degeneration. Researchers analyzed clinical trials and observational studies to explore correlations between baseline visual acuity, lesion size, growth rate, foveal involvement, and focality with changes in visual acuity over two years. Key findings reveal faster GA lesion growth correlates with greater vision loss, particularly in eyes with subfoveal or unifocal lesions. Baseline measures, like visual acuity and lesion size, do not predict vision changes. Foveal involvement significantly accelerates vision loss. The study emphasizes identifying high-risk patients and highlights the need for interventions to slow GA progression.