Posted inInteresting Papers
Increased risk of glaucoma development in patients with central serous chorioretinopathy: results of a 11-year population-based cohort study
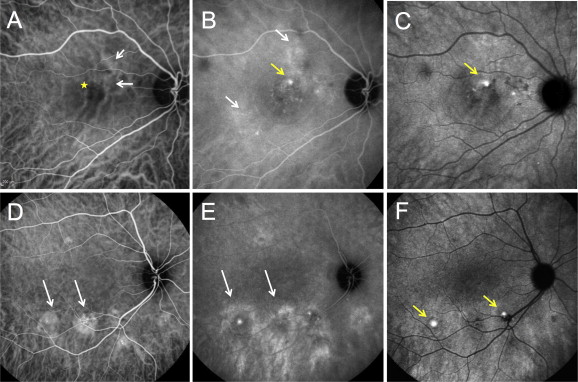
Purpose: To investigate whether patients with central serous chorioretinopathy (CSC) have increased risk of developing glaucoma. Methods: Patients diagnosed with CSC between 1 January 2008 and 31 December 2018 were included in…