Posted inInteresting Papers
Shifting Tides in Diabetic Retinopathy Treatment: The Rise of Ranibizumab and Decline of Panretinal Photocoagulation Post-Protocol S
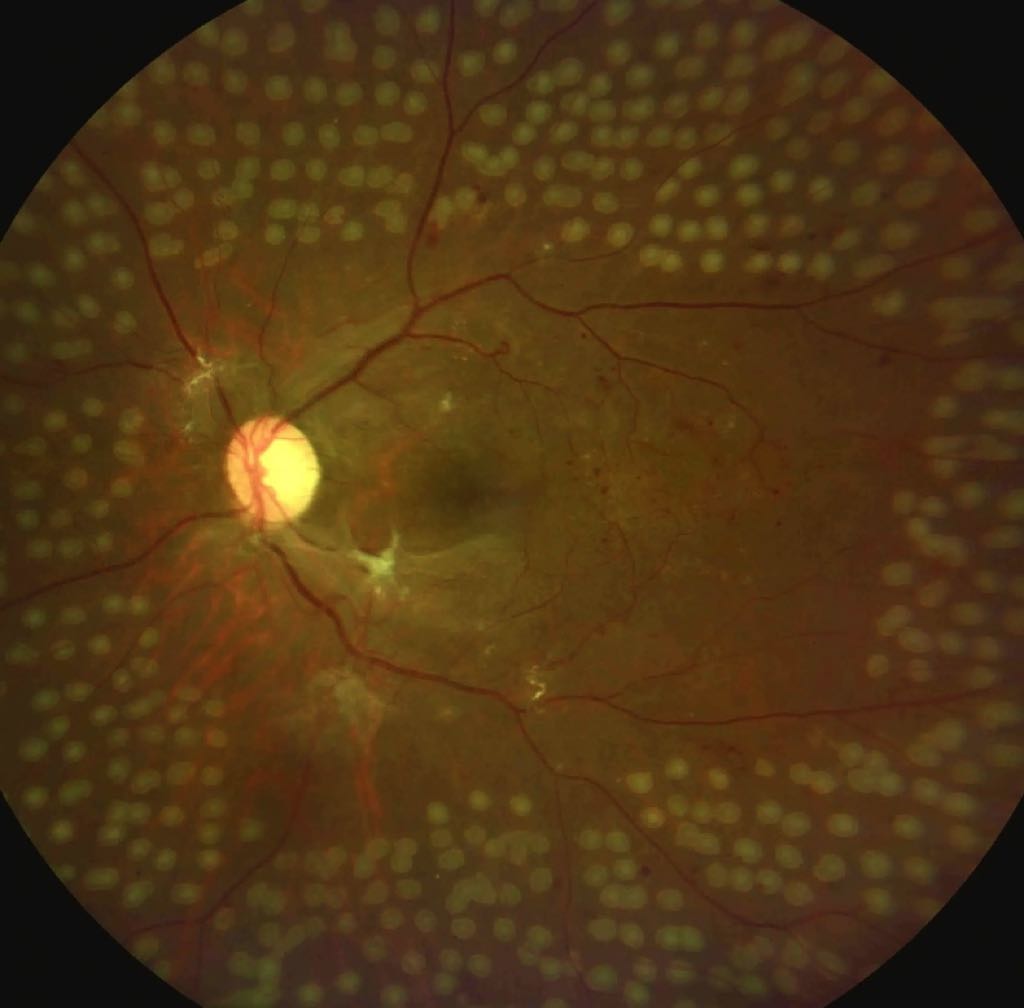
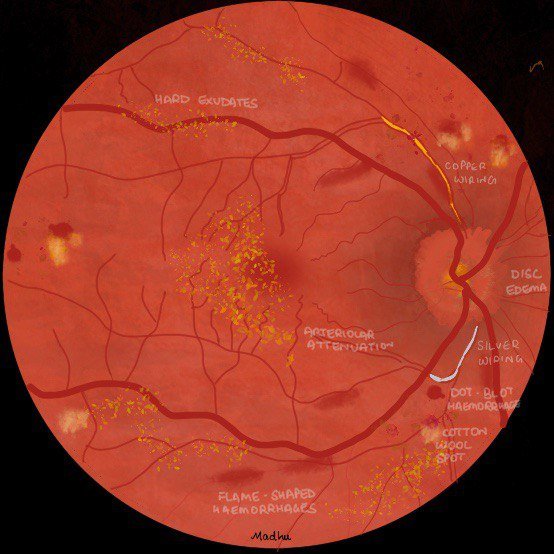
Overview of Proliferative Diabetic Retinopathy (PDR): PDR is the most advanced form of diabetic eye disease, affecting patients with type 1 and type 2 diabetes mellitus. Treatment options include…