Hydroxychloroquine Retinopathy
- Definition and Importance:
- Hydroxychloroquine (HCQ) retinopathy is a toxic ocular effect of long-term HCQ use, primarily for rheumatic (e.g., systemic lupus erythematosus [SLE], rheumatoid arthritis) and dermatologic conditions.
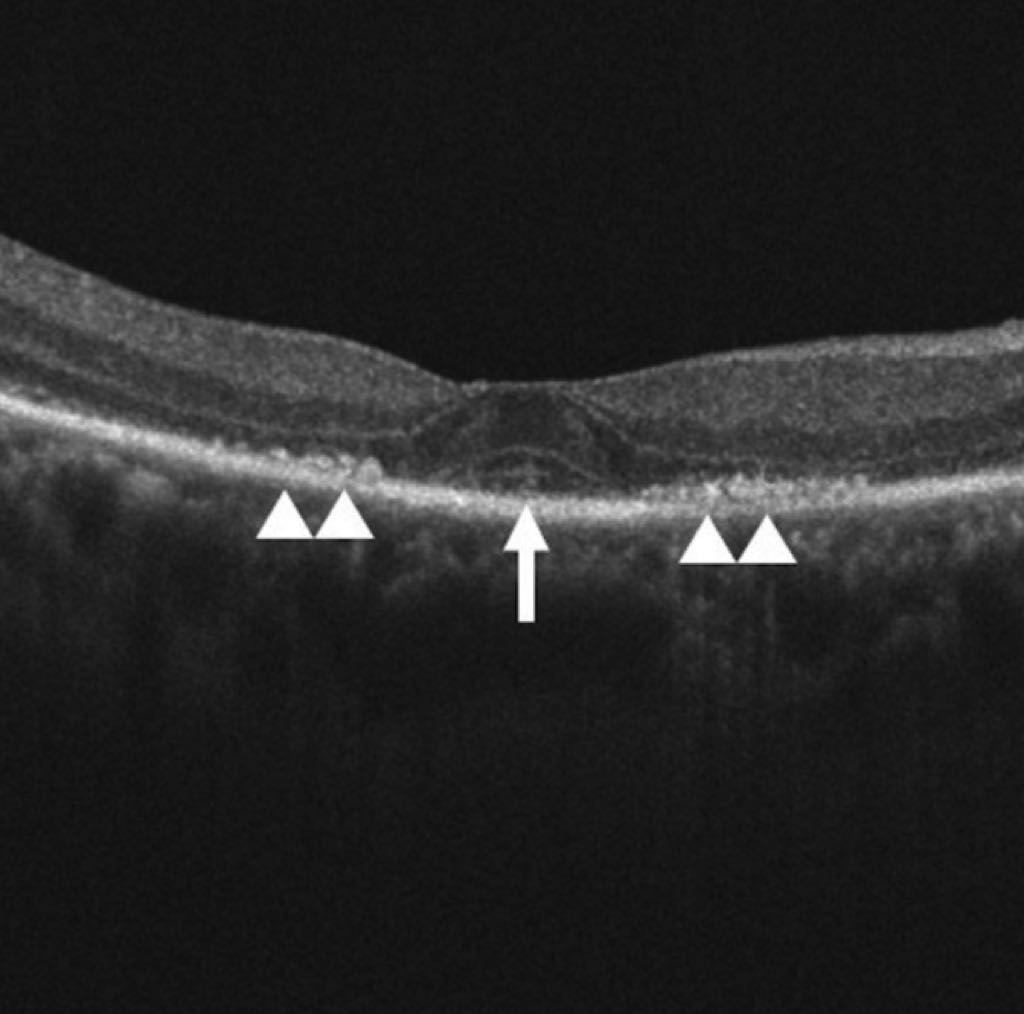
- Characterized by outer retinal thinning and retinal pigment epithelium (RPE) damage, potentially leading to vision loss in advanced stages.
- Risk is low within the first 5 years (<1%) but increases to 8.6% after 15 years of use.
- Study Overview:
- Cohort study of 4677 long-term HCQ users in Kaiser Permanente Northern California (1997–2020), with up to 15 years of follow-up.
- Incident HCQ retinopathy adjudicated via masked review of spectral domain-optical coherence tomography (SD-OCT) by expert ophthalmologists, classified as parafoveal (damage 2°–6° from fovea) or pericentral (damage ≥8° from fovea).
- Demographics:
- Mean age at HCQ initiation: 52.4 ± 14.1 years.
- 82.9% female (3877/4677), 17.1% male (800/4677).
- Race/ethnicity: 58.1% non-Hispanic White, 13.7% Asian, 10.5% Black, 17.7% Hispanic.
- 11.5% had chronic kidney disease (CKD) stage ≥3 after 5 years.
- Key Risk Factors for HCQ Retinopathy:
- Older Age at Initiation:
- Compared to <45 years (reference):
- 45–54 years: Adjusted HR 2.48 (95% CI, 1.28–4.78).
- 55–64 years: Adjusted HR 3.82 (95% CI, 2.05–7.14).
- ≥65 years: Adjusted HR 5.68 (95% CI, 2.99–10.79).
- Likely due to age-related retinal thinning increasing susceptibility.
- Compared to <45 years (reference):
- Female Sex:
- Adjusted HR 3.83 (95% CI, 1.86–7.89) vs. males.
- Males had <3% cumulative incidence over 15 years.
- Biological basis unclear, but sex disparities noted in other retinal conditions.
- Chronic Kidney Disease (CKD) Stage ≥3:
- Adjusted HR 1.95 (95% CI, 1.25–3.04).
- Risk increases with lower eGFR (<60 mL/min/1.73 m²), as HCQ undergoes 25%–40% renal clearance, leading to higher systemic exposure.
- Tamoxifen Use:
- Adjusted HR 3.43 (95% CI, 1.08–10.89), despite only 18 users (3 cases).
- Potential synergistic retinal toxicity with HCQ.
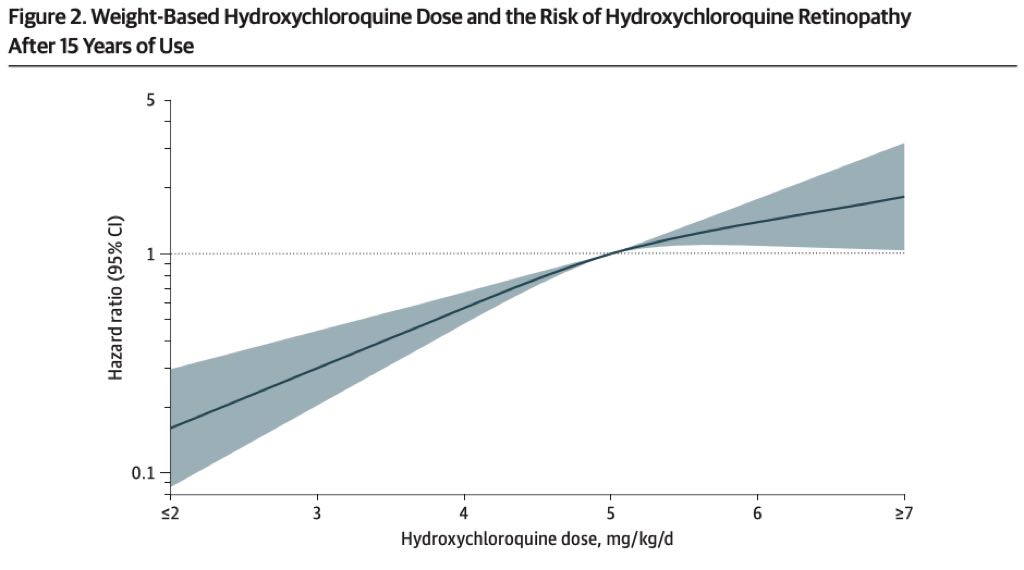
- HCQ Dose:
- Higher weight-based dose at 5 years increased risk:
- ≤5 mg/kg/day: Reference.
- 5–6 mg/kg/day: Adjusted HR 3.23 (95% CI, 1.90–5.50).
-
6 mg/kg/day: Adjusted HR 5.30 (95% CI, 3.46–8.10).
- Linear dose-response relationship (no safe threshold); lowest effective dose recommended.
- Cumulative Dose:
- Per 100 g increase in first 5 years: Adjusted HR 1.64 (95% CI, 1.44–1.87).
- Cumulative Dose:
- Higher weight-based dose at 5 years increased risk:
- Older Age at Initiation:
- Race/Ethnicity and Retinopathy Patterns:
- Overall HCQ retinopathy risk not significantly associated with race/ethnicity.
- Pericentral Pattern:
- Higher in Asian patients: Adjusted HR 15.02 (95% CI, 4.82–46.87) vs. non-Hispanic White.
- 54.2% of Asian cases (13/24) were pericentral vs. 5.3% (4/76) in non-Hispanic White.
- Higher in Black patients: Adjusted HR 5.51 (95% CI, 1.22–24.97).
- 60% of Black cases (3/5) were pericentral.
- Hispanic patients: No significant difference (15% pericentral, 3/20 cases).
- Higher in Asian patients: Adjusted HR 15.02 (95% CI, 4.82–46.87) vs. non-Hispanic White.
- Parafoveal Pattern:
- Associated with older age (≥55 years: Adjusted HR 3.05, 95% CI, 1.98–4.71), female sex (Adjusted HR 5.50, 95% CI, 2.23–13.59), and CKD stage ≥3 (Adjusted HR 1.92, 95% CI, 1.18–3.12).
- Black race associated with lower risk (Adjusted HR 0.22, 95% CI, 0.05–0.88).
- Non-Significant Risk Factors:
- Cytochrome P450 (CYP) inhibitor use (e.g., CYP2D6, CYP2C8, CYP3A4): Adjusted HR 0.67 (95% CI, 0.39–1.13).
- Diabetes, liver disease, and indication for HCQ use (SLE/CTD, rheumatoid arthritis, dermatologic) not associated with increased risk.
- Clinical Implications:
- Dosing: Use lowest effective dose (<5 mg/kg/day ideal) to minimize risk, especially in high-risk groups (older age, female, CKD, tamoxifen users).
- Screening:
- Annual screening recommended after 5 years of use, using SD-OCT and visual fields.
- Pericentral pattern requires wider fundus examination (e.g., 24-2 or 30-2 visual fields) due to its peripheral location, especially in Asian and Black patients.
- Early detection critical, as retinopathy is often asymptomatic until advanced stages.
- Individualized Care: Adjust dosing and screening frequency based on risk factors (e.g., closer monitoring for older females with CKD or tamoxifen use).
- Strengths of Study:
- Large cohort (4677 patients) with diverse racial/ethnic representation.
- Long-term follow-up (up to 15 years).
- Accurate HCQ exposure via pharmacy records (accounts for adherence).
- Masked SD-OCT adjudication by experts, reducing misclassification bias.
- Limitations:
- No data on HCQ blood levels, which may correlate with retinopathy risk.
- Asymptomatic nature of early retinopathy may delay onset detection.
- Small number of pericentral cases (23/125) limited power for subtype analysis.
- Few tamoxifen users (18) and Black patient cases (5), requiring replication for these findings.
- Key Takeaways for Exams:
- Major risk factors: Older age, female sex, CKD stage ≥3, tamoxifen use, higher HCQ dose (>5 mg/kg/day), and cumulative dose.
- Pericentral pattern strongly associated with Asian and Black race/ethnicity, requiring wider screening fields.
- Screening modalities: SD-OCT is gold standard; ensure wide-field testing for pericentral pattern in at-risk groups.
- Management: Use lowest effective dose, monitor high-risk patients closely, and educate on importance of annual screening after 5 years.
Citation
Jorge AM, Melles RB, Marmor MF, et al. Risk Factors for Hydroxychloroquine Retinopathy and Its Subtypes. JAMA Network Open. 2024;7(5):e2410677. doi:10.1001/jamanetworkopen.2024.10677