Choroidal Vasculitis and Indocyanine Green Angiography (ICGA)
– Definition and Importance of Choroidal Vasculitis:
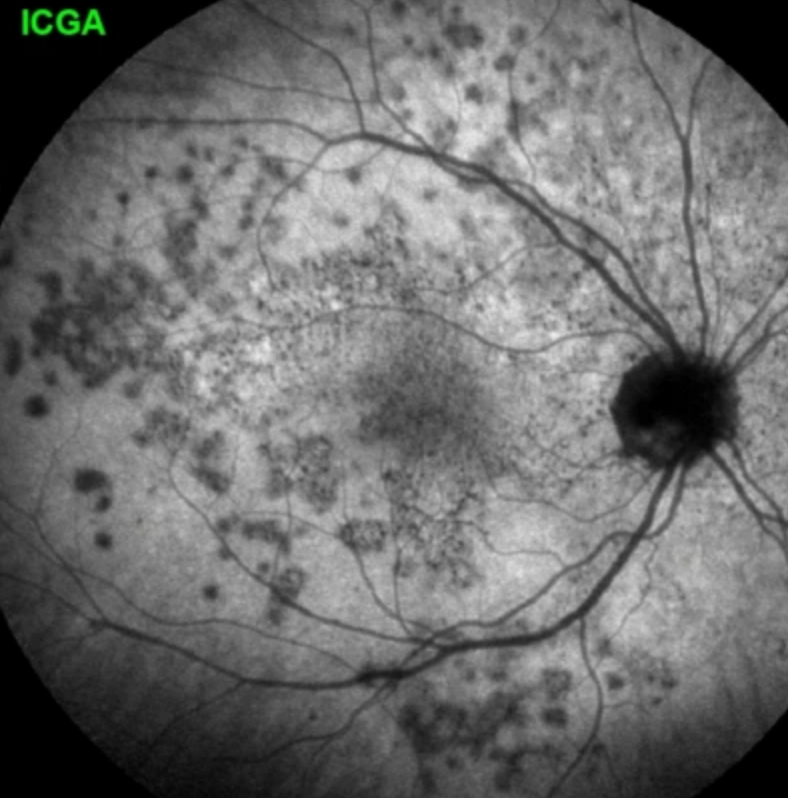
– Choroidal vasculitis is a hallmark of choroidal inflammation, often underdiagnosed without ICGA.
– ICGA is the gold standard for diagnosing and monitoring choroidal vasculitis, providing precise visualization of choriocapillaris and stromal involvement.
– Divided into two main types: choriocapillaritis (occlusive) and stromal choroidal vasculitis (leaky).
– Indocyanine Green Angiography (ICGA) Principles:
– Utilizes indocyanine green (ICG) molecule, which fluoresces at ~830 nm, penetrating retinal pigment epithelium (RPE) for choroidal visualization.
– ICG binds to blood proteins (98%), forming large complexes (60,000–80,000 Daltons), preventing leakage from retinal or large choroidal vessels but egressing physiologically from fenestrated choriocapillaris.
– Key ICGA patterns:
– Choriocapillaritis: Hypofluorescent areas indicating non-perfusion (dots to geographic areas).
– Stromal choroiditis: Hyperfluorescent leaky vessels, fuzzy vessels, and late diffuse hyperfluorescence.
– Choroidal Anatomy and Blood Flow:
– Choroid is the most vascularized ocular tissue with high blood flow per gram.
– Arterial supply via ophthalmic artery → ciliary arteries → choriocapillaris (fenestrated endothelium).
– Venous drainage through vortex veins (3–8 per eye, typically 4–5).
– Choriocapillaris is a lobular mesh with central arteriolar feeders and peripheral draining venules.
– Choriocapillaritis (Primary and Secondary):
– Multiple Evanescent White Dot Syndrome (MEWDS):
– Mildest form, affects end-capillary choriocapillaris.
– ICGA: Small, non-confluent hypofluorescent dots, more visible in late phases.
– Usually unilateral, self-resolving, no scarring.
– OCT-A often normal due to insensitivity to low-flow vessels.
– Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPPE):
– Involves larger choriocapillaris vessels, causing confluent hypofluorescent areas on ICGA.
– Bilateral, may require corticosteroids for macular involvement.
– Associated with cerebral vasculitis in some cases.
– Idiopathic Multifocal Choroiditis (MFC):
– Recurrent, bilateral, leads to chorioretinal scars and choroidal neovascularization (CNV) in ~30% of cases.
– ICGA findings similar to MEWDS initially but progressive with scarring.
– Requires aggressive immunosuppression.
– Serpiginous Choroiditis (SC):
– Most severe, involves larger choriocapillaris/pre-capillary arterioles, causing creeping hypofluorescent patterns.
– Idiopathic or tuberculosis-related (requires IGRA testing).
– Needs dual/triple immunosuppression to halt progression.
– Secondary Causes:
– Acute Syphilitic Posterior Placoid Chorioretinitis (ASPPC): Immunologic reaction causing choriocapillaris non-perfusion, treatable with antibiotics and corticosteroids.
– Tuberculosis-related SC: Extensive non-perfusion, responsive to anti-tuberculous therapy and immunosuppression.
– Stromal Choroidal Vasculitis:
– Characterized by hyperfluorescent signs on ICGA:
– Early hyperfluorescent vessels.
– Fuzzy/indistinct vessels in intermediate phase.
– Late diffuse choroidal hyperfluorescence, often obscuring hypofluorescent dark dots (HDDs).
– Primary Conditions:
– Vogt-Koyanagi-Harada (VKH) Disease:
– Autoimmune stromal inflammation, evenly distributed HDDs on ICGA.
– Additional signs: disc hyperfluorescence, pinpoint leaks causing serous retinal detachments.
– Severe, requires high-dose corticosteroids.
– Sympathetic Ophthalmia (SO): Similar to VKH but triggered by ocular trauma/surgery, less severe.
– HLA-A29 Birdshot Retinochoroiditis (BRC):
– Involves both retina and choroid, less severe than VKH.
– ICGA shows HDDs, minimal early vessel hyperfluorescence, and fading HDDs in late phases.
– Secondary Conditions:
– Ocular sarcoidosis: Variable severity, uneven HDDs, may include macroaneurysms.
– Systemic lupus erythematosus (SLE): Occlusive vasculitis of large choroidal vessels, Amalric’s triangular sign on ICGA.
– Giant Cell Arteritis (GCA):
– Occlusion of posterior ciliary arteries (PCA), causing triangular choroidal non-perfusion (Amalric’s sign).
– Associated with anterior ischemic optic neuropathy (AION).
– Ophthalmic emergency requiring immediate corticosteroids.
– Scleritis-related: Choroidal vasculitis in 57% of posterior scleritis cases.
– ICGA Semiology:
– Normal ICGA:
– Intermediate phase (8–11 min): Vessels fluorescent (dye intravascular).
– Late phase (>20 min): Vessels dark (dye in stroma), faint background fluorescence from physiological ICG leakage.
– Pathologic Signs:
– Choriocapillaritis: Hypofluorescent dots (MEWDS) or geographic areas (APMPPE, MFC, SC).
– Stromal vasculitis: Fuzzy vessels, hyperfluorescent vessels, late diffuse hyperfluorescence, HDDs (space-occupying lesions blocking ICG diffusion).
– HDDs in stromal choroiditis:
– Evenly distributed in VKH/BRC (primary).
– Uneven, irregular in sarcoidosis (secondary).
– Complementary Imaging Modalities:
– Fluorescein Angiography (FA):
– Limited to retinal vasculature, glimpses choriocapillaris in first 60 seconds.
– Useful for APMPPE (early hypofluorescence) and retinal vasculitis in BRC.
– Spectral Domain OCT (SD-OCT) and Enhanced Depth Imaging (EDI-OCT):
– Detects outer retinal damage in choriocapillaritis (photoreceptor loss).
– EDI-OCT visualizes choroidal thickening (VKH) and granulomas (sarcoidosis).
– OCT Angiography (OCT-A):
– Non-invasive, detects flow in larger choriocapillaris vessels (APMPPE, MFC, SC).
– Limited for end-capillary flow (MEWDS) and stromal choroiditis.
– Fundus Autofluorescence (FAF):
– Hyperautofluorescence in choriocapillaritis due to RPE/photoreceptor damage.
– Less useful in early stromal choroiditis.
– Therapeutic Implications:
– Choriocapillaritis:
– MEWDS: Often no treatment needed.
– APMPPE: Corticosteroids for severe cases.
– MFC/SC: Aggressive immunosuppression to prevent scarring/CNV.
– Stromal Choroiditis:
– VKH/SO: High-dose corticosteroids, often intravenous.
– BRC: Immunosuppression tailored to severity.
– GCA: Immediate high-dose corticosteroids to prevent bilateral vision loss.
– Secondary causes (e.g., TB, syphilis): Treat underlying infection alongside inflammation.
– Historical Context and Misnomers:
– Terms like “white dot syndromes” are outdated, grouping unrelated diseases by fundus appearance.
– ICGA clarified pathophysiology (e.g., APMPPE as choriocapillaritis, not RPE disease).
– Deutman’s term “Acute Multifocal Ischaemic Choriocapillaritis (AMIC)” for APMPPE was prescient, later validated by ICGA.
– Diagnostic Pitfalls:
– Overreliance on OCT-A: Misses end-capillary non-perfusion (e.g., MEWDS).
– Neglecting ICGA: Leads to missed choroidal vasculitis, especially in stromal choroiditis.
– Misinterpreting FA: Limited to retinal/choriocapillaris glimpse, inadequate for stromal assessment.
Citation
Papasawvas, I., Tucker, W. R., Mantovani, A., Fabozzi, L., & Herbort, C. P. Jr. (2024). Choroidal vasculitis as a biomarker of inflammation of the choroid. Indocyanine Green Angiography (ICGA) spearheading for diagnosis and follow-up, an imaging tutorial. *Journal of Ophthalmic Inflammation and Infection*, 14(63). https://doi.org/10.1186/s12348-024-00442-w