Age-related macular degeneration (AMD) remains a leading cause of vision loss worldwide, and catching its progression early is critical for preserving sight. A fascinating new study, published in the American Journal of Ophthalmology (February 2025), dives into the nitty-gritty of how we detect early macular atrophy—a precursor to geographic atrophy (GA)—using advanced imaging techniques. Led by researchers like Yuxuan Cheng, Monika Fleckenstein, Philip J. Rosenfeld, and others from top institutions such as the Moran Eye Center, Bascom Palmer Eye Institute, and Tel Aviv Medical Center, this paper compares two optical coherence tomography (OCT) approaches: traditional B-scans and en face imaging. The findings? They could reshape how we diagnose and monitor AMD.
What’s the Big Question?
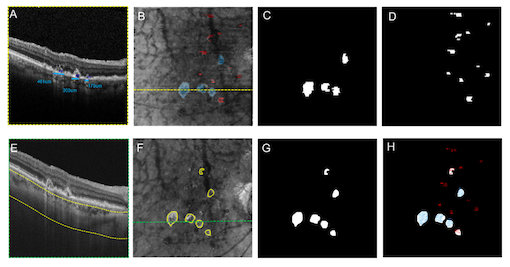
In AMD, the retina’s outer layers and retinal pigment epithelium (RPE) can degrade, leading to atrophy and, eventually, GA—a severe, irreversible stage. To catch this process early, experts use terms like complete RPE and outer retinal atrophy (cRORA) and incomplete RPE and outer retinal atrophy (iRORA), defined by OCT B-scan features like photoreceptor loss and choroidal hypertransmission defects (hyperTDs). Meanwhile, en face OCT imaging offers a bird’s-eye view of these hyperTDs, potentially spotting atrophy in any direction—not just horizontally. So, which method is better at nailing down these early changes?
The Study Setup
The team studied 19 eyes from 15 patients with nonexudative (dry) AMD, all showing signs of GA. Each eye got same-day scans using two cutting-edge tools:
- Spectral-domain OCT (SD-OCT): Produced detailed B-scans (97 per eye, spaced 62 µm apart) to grade cRORA and iRORA.
- Swept-source OCT angiography (SS-OCTA): Generated en face images from a sub-RPE slab (64–400 µm below Bruch’s membrane) to spot persistent hyperTDs.
Graders at different centers analyzed the images. B-scans were checked for cRORA (hyperTDs ≥250 µm) and iRORA (<250 µm), while en face images flagged hyperTDs of any orientation ≥250 µm. Then, they compared the results.
Key Findings: A Near-Perfect Match—and a Twist
Here’s where it gets exciting:
- cRORA and HyperTDs Align Almost Perfectly: A whopping 99.6% of cRORA lesions on B-scans matched persistent hyperTDs on en face images. Areas measured on both systems were nearly identical (1.98 mm² for cRORA vs. 2.14 mm² for hyperTDs), with no significant difference (P = .148). This suggests en face hyperTDs are a rock-solid stand-in for cRORA—a big win for consistency.
- iRORA’s Hidden Story: About 27.4% of lesions labeled iRORA on B-scans (because they were <250 µm horizontally) turned out to be part of larger hyperTDs on en face images. Why? B-scans only measure horizontally, missing bigger lesions in other directions. Even with neighboring B-scans considered, some iRORA was really cRORA in disguise.
Why This Matters
En face imaging could be a game-changer. Unlike B-scans, which require scrolling through dozens of slices, en face gives a single, comprehensive view—faster and easier to interpret. It also catches atrophy in any dimension, not just horizontal, reducing the chance of misclassifying iRORA as less severe than it is. Plus, automated algorithms (used here with SS-OCTA) make spotting hyperTDs a breeze, boosting efficiency.
For clinicians and researchers, this means:
- Better Monitoring: En face OCT could track AMD progression more reliably, especially in clinical trials.
- Real-World Impact: A single scan could assess both dry and wet AMD, streamlining patient care.
The Catch
The study’s sample size was small (19 eyes), but the strong overlap between cRORA and hyperTDs suggests more eyes wouldn’t shift the core findings. Also, the tech here—dense scan patterns and fancy algorithms—needs high-end OCT systems, which might not be everywhere yet. Still, the authors recommend at least 97 B-scans over a 6×6-mm area for accurate grading, a feasible target for modern devices.
Takeaway for Retina Enthusiasts
This paper shines a light on en face OCT’s potential to simplify and sharpen early atrophy detection in AMD. While B-scans remain vital for detailed structural views, en face imaging offers a practical, panoramic alternative—especially for spotting those sneaky lesions that look small one way but loom larger in another. As we push for earlier interventions in AMD, studies like this pave the way for smarter diagnostics.
Want to dive deeper? Check out the full paper in the American Journal of Ophthalmology (Vol. 270, February 2025). It’s a must-read for anyone keen on the future of retinal imaging!