Central serous chorioretinopathy is a chorioretinal disease characterized by a serous neuroretinal detachment in the active disease stage. This neuroretinal detachment is associated with defects in the retinal pigment epithelial layer’s outer blood-retina barrier, which occur above corresponding abnormalities in the choroid. Symptoms of CSC typically include impaired and/or distorted central vision together with altered color perception, and the disease is often associated with reduced vision-related quality of life. CSC is generally more common among men and has a typical age of onset ranging between 35 and 50 years, although it has been reported to occur at as early as 7 years of age and as late as 83 years of age. After neovascular age-related macular degeneration, diabetic macular edema, and retinal vein occlusion, CSC is the fourth most common retinopathy that causes macular fluid leakage. Although the subretinal fluid can resolve spontaneously in CSC, its course can also be complicated, resulting in atrophy of the retinal pigment epithelium and/or photoreceptors, as well as secondary macular neovascularization. Although the pathophysiology of CSC remains poorly understood, choroidal abnormalities appear to play a key role.
CSC was first described by Von Graefe in 1866 as “relapsing central luetic retinitis“. In the 1940s, Duke-Elder renamed the condition “central serous retinopathy”. The SRF leakage was subsequently believed to be caused by spasms of the retinal vessels, and in 1955 Bennett was the first to report that patients with central serous retinopathy had a high incidence of stress disorders, stressful life situations, and what he called a “tense obsessional mental make-up“. In 1965, Maumenee observed that CSC was associated with leakage at the level of the RPE, not from the retinal vessels; a few years later, Maumenee and his colleagues proposed that laser treatment might be effective for treating this leakage. Subsequently, Gass hypothesized that increased hyperpermeability of the choriocapillaris causes increased hydrostatic pressure, causing retinal pigment epithelial detachments and defects in the RPE outer blood-retina barrier, allowing fluid to leak into the subretinal space. This theory was confirmed years later after the introduction of indocyanine green angiography and optical coherence tomography.
Recently, the incidence of CSC was studied in a population-based longitudinal cohort study using a nationwide database of health insurance claims collected over an 8-year period by the Japanese Ministry of Health, Labour, and Welfare. The authors found that the incidence of CSC among individuals in the general population 30 years of age and older was 34.0 per 100,000 person-years. Remarkably, they also found that this incidence was nearly 3.5-fold higher in men than in women (54.2 versus 15.7 per 100,000 person-years, respectively). In contrast, a previous population-based study of a predominantly Caucasian population conducted in the US found lower annual age-adjusted rates of CSC in 1980 through 2002, with an incidence of 9.9 and 1.7 per 100,000 men and women, respectively. Notably, among patients taking oral corticosteroid, an annual incidence of 54.5 and 34.2 per 100, 000 men and women, respectively, was reported in a population-based study conducted in Taiwan. Another cohort study conducted among users of any type of corticosteroids in South Korea found an incidence of CSC of 54 and 16 per 100,000 person-years in men and women, respectively. Although these differences in the reported incidence of CSC may be due in part to ethnic, socio-demographic, and/or methodological differences, these rates may be an underestimation. For example, Kitzmann and colleagues excluded patients for whom fluorescein angiography data were not available. Moreover, these studies lacked widefield fundus autofluorescence imaging, which can reveal otherwise clinically unrecognized gravitational tracts. Lastly, the incidence reported by some studies was based on data regarding insurance claims.
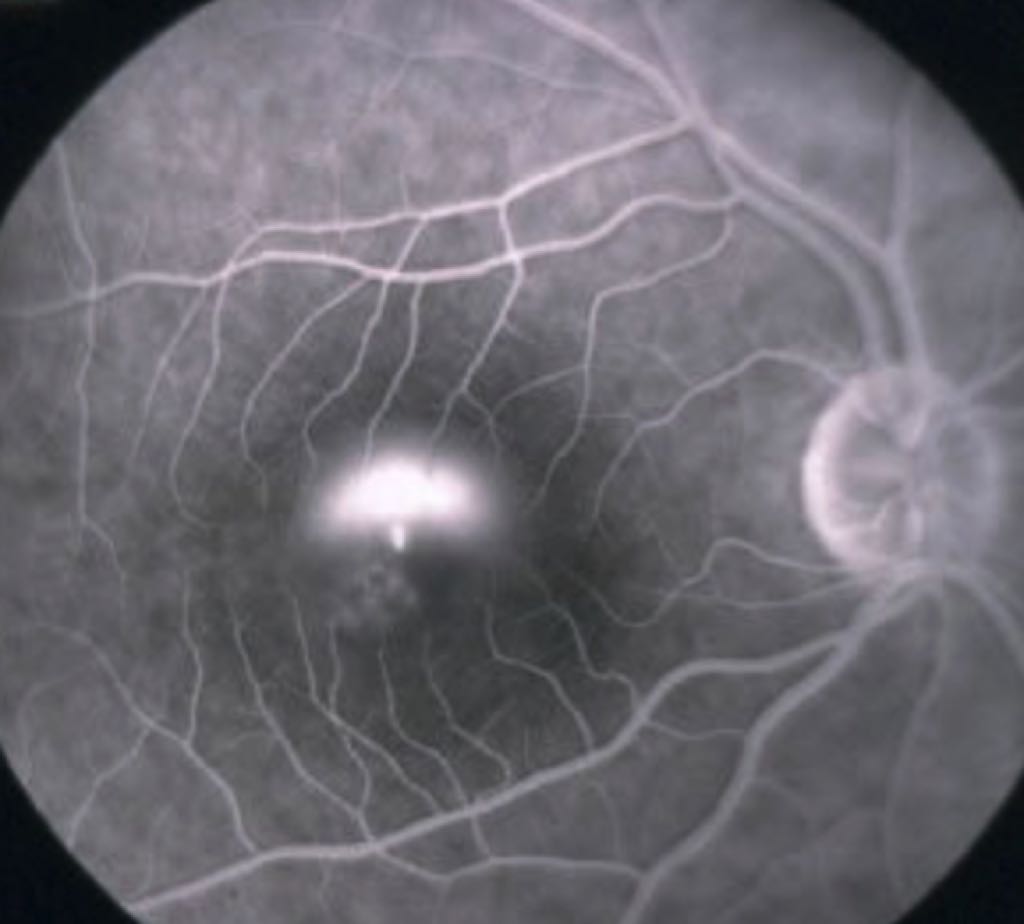
Multimodal imaging modalities, including OCT, FA, ICGA, and FAF, are important for establishing a diagnosis of CSC, as many other conditions can mimic CSC. The presence of SRF, as well as increased choroidal thickness, serous PEDs, and dilated choroidal veins, can be evaluated using OCT. FAF can show the extent of associated outer retinal and RPE alterations, while FA can detect leakage of fluid into the subretinal space, a characteristic feature of CSC. In addition, choroidal abnormalities characteristic of CSC can be appreciated easily on ICGA. Finally, MNV can be detected using a combination of OCT, OCT angiography, FA, and ICGA, although conclusively detecting MNV can be challenging.
Until recently, the preferred treatment for CSC was somewhat controversial, due to a lack of large prospective randomized treatment trials and relatively few large retrospective studies. Evidence-based treatment of CSC is complicated by a large number of retrospective studies that do not provide adequate information or lack sufficient power, including small sample size, no control group, variable and/or questionable inclusion criteria, and inadequate techniques for quantitatively assessing OCT findings.
Retrospective studies are particularly problematic in CSC, as spontaneous resolution of SRF is common not only in acute CSC, but even in clinical trials; for example, in the VICI trial 30 % of placebo-treated patients with chronic CSC had complete resolution of SRF on OCT after 1 year of follow-up.
Thus, retrospective studies of CSC have resulted in many scientifically questionable claims regarding treatment efficacy, in which the presumed treatment effect may have been largely due of the disease’s waxing-and-waning nature. In recent years, however, several important steps have been made in order to provide sufficient information to support an evidence-based treatment guideline for CSC.
The results obtained from 3 large, randomized controlled trials—namely, the PLACE trial, the aforementioned VICI trial, and the SPECTRA trial—showed the superiority of half-dose photodynamic therapy over high-density subthreshold micropulse laser treatment, non-superiority of the oral mineralocorticoid receptor antagonist eplerenone treatment compared to placebo, and superiority of half-dose PDT over eplerenone treatment. In addition, the results of long-term follow-up studies, as well as crossover studies, support the beneficial role of PDT in the treatment of CSC.
Clinical characteristics of central serous chorioretinopathy
The classification of CSC remains controversial. Several classification systems for CSC and subtypes of CSC have been proposed, but to date no universal classification has been accepted, and ophthalmologists disagree with respect to the classification of CSC. However, a distinction between acute and chronic forms of CSC is commonly used, based predominantly on the duration of SRF and the structural changes visible on multimodal imaging. With aCSC, SRF usually resolves spontaneously within 3-4 months, without the need for treatment. In contrast, with CCSC the SRF generally persists for more than 3-4 months, and may lead to permanent structural neuroretinal and RPE damage, as well as subsequent long-term vision loss and decreased vision-related quality of life. In addition, some patients with cCSC may report a relatively recent disease onset even though findings on multimodal imaging are indicative of prolonged disease. Furthermore, in the acute versus chronic CSC classification system, aCSC is often characterized by an isolated dome-shaped neuroretinal detachment on OCT, fewer leakage points on FA, and limited atrophic RPE changes on multimodal imaging. In contrast, cCSC is distinguished by more extensive leakage on FA, and the chronic leakage of SRF tends to case a shallower neuroretinal detachment compared to aCSC. However, some patients with CSC present with one or more leaks on FA that persist for longer than 4 months but are not associated with widespread RPE abnormalities; these cases are therefore difficult to classify using the current aCSC/CCSC classification system. The classification of CSC is discussed in further detail in Section 1.1.3.
The term “focal leakage point” typically describes a single point of expanding hyperfluorescence on FA, whereas “diffuse leakage” describes the presence of multiple focal leakage points or ill-defined areas of leakage. The leakage of fluorescein through a single defect in the RPE causes a focal leakage point on early phase FA, which typically increases in size and has indistinct borders in later phases of FA. The focal area of leakage on FA often co-localizes with a corresponding PED visible on OCT.
Importantly, a PED is presumed to be the point of least resistance at the RPE outer blood-retina barrier due to increased vascular pressure from the choriocapillaris, which then causes increased wall stress and damage. This small opening in the RPE facilitates leakage into the subretinal space.
Distinguishing between clinical subtypes of CSC is important for determining the optimal treatment strategy. Although the terms aCSC and CCSC are clearly too simplistic to classify CSC adequately, they are widely used in the literature when discussing the disease course and treatment of CSC, and are therefore used in this review as well. Nevertheless, attempts are being made to refine the classification of CSC, for which further validation is needed.
Acute CSC
Acute CSC is characterized by a relatively recent onset of serous neuroretinal detachment, often involving the macula. In most cases, the SRF resolves spontaneously within 3-4 months following onset, and patients with aCSC typically have a good visual prognosis. A study of 31 patients with aCSC conducted in pre-OCT era showed spontaneous, complete SRF resolution in 84% of cases after 6 months of follow-up. Another study involving 27 patients with presumed aCSC found that SRF resolved spontaneously in 100 % of patients after a mean follow-up of 23 months.
On the other hand, a recurrence of SRF has been reported in up to 52% of patients with aCSC.
In a retrospective study of 295 affected eyes in 291 patients with aCSC, of which 154 eyes had spontaneous SRF resolution and 141 had SRF resolution after treatment, Mohabati and colleagues found that SRF recurred in 24% of untreated cases and 4% of treated cases (most of which were treated using PDT). In addition, some studies have shown that even a brief period of SRF can still cause irreversible photoreceptor damage; thus, relatively early treatment may also be indicated in aCSC cases.
Several risk factors for prolonged CSC duration at presentation have been proposed, including
- subfoveal choroidal thickness exceeding 500 µm,
- PED > 50 µm,
- presentation at 40 years of age or older, and
- photoreceptor atrophy in the area of the detached neuroretina combined with granular debris in the SRF on OCT.
Moreover, a larger volume of SRF in aCSC has been suggested to cause more photoreceptor damage. These risk factors, as well as the patient’s clinical profile, profession, and preference, can affect the treating physician’s choice of whether or not to treat patients with aCSC who present with SRF.
Together with a dome-shaped neuroretinal detachment in aCSC, hyperreflective dots may also be present on FAF and correspond to small white dots visible on ophthalmoscopy. These dots can represent RPE cells, photoreceptor outer segments, and/or macrophages and can migrate progressively into the neuroretina in patients with a prolonged disease course. However, these dots have also been suggested to represent plasma proteins derived from the choriocapillaris and/or inflammatory debris.
Fibrinogen can also leak through the RPE and may—in rare cases—appear on OCT as a presumed fibrin clot.
In addition, a recent study found that patients who present with subretinal fibrin generally had a worse mean baseline BCVA (best-corrected visual acuity) compared to patients without subretinal fibrin.
In aCSC, up to 1-3 focal leakage points are typically visible on FA. The most common pattern of leakage on FA is described as “inkblot” leakage. This focal leak appears during dye transit and becomes increasingly less-defined as the dye leaks more slowly into the subretinal space through the RPE defect. Another characteristic leakage pattern on FA in aCSC is known as a “smokestack” leakage, which includes a focal hyperfluorescent pinpoint with an expanding area of hyperfluorescence over time. Smokestack leakage on FA can be associated with a larger serous detachment compared to inkblot leakage. The location of the focal leakage point is usually correlated with a micro-tear in the RPE, and in aCSC this finding typically occurs in the absence of more diffuse atrophy of the RPE.
Areas of focal indistinct hyperfluorescent leakage on ICGA—corresponding to dye leakage due to choroidal vascular hyperpermeability—are characteristic in CSC and are often best visible on mid-phase ICGA. These findings generally correspond to areas in which focal leakage is apparent on FA. In CSC, hyperfluorescent areas on ICGA are generally more widespread than the hyperfluorescent areas on FA, as the primary affected tissue in CSC appears to be the choroid.
With aCSC, areas of decreased autofluorescence on FAF have been found to overlap with attenuation of RPE and areas of leakage on FA. Because FAF reflects the functional and structural status of the RPE, this finding is another indicator that the RPE plays a role in the pathophysiology of CSC.
In the absence of significant RPE damage, areas of current or prior SRF typically show as hyperautofluorescence on FAF, due to the increased signal contribution from the RPE.
Some groups consider non-resolving CSC to be a variant of aCSC characterized by persistent SRF lasting at least 4 months with no accompanying RPE abnormalities. Alternatively, recurrent CSC is another variant of aCSC described as one or more episodes of SRF after complete resolution of the first episode of SRF in aCSC. However, these variants clearly have clinical overlap, and what may constitute “cCSC” depends largely on the definition used. Lastly, some cases that appear as aCSC on presentation can develop features consistent with cCSC, making a clear definition and classification system difficult.
Chronic CSC
Chronic CSC is characterized by a persistent serous neuroretinal detachment, which can be either small in size or extensive, as well as multifocal in the case of multiple leakage areas; cCSC typically presents with atrophic RPE changes on FA that can range from a single localized area to extensively diffuse atrophic RPE alterations. With cCSC, SRF on OCT typically persists for longer than 3-4 months, and one or more focal leakage points are visible on FA. In some cases, clearly identifiable leakage points may be either absent or difficult to identify against the background of irregular RPE “window” defects. The presence of SRF without focal leakage may be indicative of resolving CSC and may appear together with certain signs on OCT such as the so-called “Fuji sign” (an accumulation of SRF on OCT that has the appearance of Mount Fuji in Japan and has been associated with spontaneous resolution).The Fuji sign was considered to be present when the external limiting membrane was positioned either exactly overlapping the 2 legs of the triangle or under these lines.
With cCSC, widespread abnormalities on ICGA are typically observed and may include dilated choroidal veins, delayed choroidal filling, and/or choroidal vascular hyperpermeability. Patients with typical cCSC typically present with one or more areas of indistinct mid-phase hyperfluorescence on ICGA.
Although there are currently no strict definitions of severe and non-severe CSC, a distinction between complex CSC and simple CSC has been suggested, with complex CSC defined as the presence of a total area of RPE alterations involving an area of more than twice the size of the optic disc. However, to date no conclusive evidence exists to suggest that this definition of complex CSC translates to increased severity in terms of clinical outcome.
Interestingly, patients with a history of typical aCSC who present with a severe cCSC phenotype are rare, indicating distinct differences between these disease presentations. Moreover, with respect to visual outcome the prognosis can differ between aCSC and cCSC. Nonetheless, aCSC, non-severe cCSC, and severe cCSC all appear to have common genetic risk factors and similarities on multimodal imaging, indicating pathophysiological overlap among these clinical entities. Indeed, a retrospective study by Castro-Correia and colleagues found that up to 50 % of patients with unspecified CSC developed atrophic RPE changes within 12 years of presentation. In addition, a long-term follow-up study of 61 aCSC cases by Mohabati et al. found that 36% of patients had a tendency toward chronic disease in terms of increased RPE changes over time, while 23% of patients had both an increase in RPE alterations over time and recurrent SRF.
PEDs on OCT have been reported in 56-96 % of affected eyes in patients with CSC. Virtually all patients with cCSC present with DARA (diffuse atrophic RPE alterations) to some extent, possibly due to the prolonged presence of SRF, previous episodes of SRF, or the result of an underlying choroidal dysfunction that directly affects the RPE, similar to pachychoroid pigment epitheliopathy.
Gravitational tracts are defined as areas of RPE and photoreceptor outer segment atrophy, corresponding hyperfluorescent RPE window defects on FA, and mixed hyperautofluorescence and hypo-autofluorescence on FAF that typically extend in the inferior direction to the prominent current or previous points of leakage. Gravitational tracts are believed to develop due to the prolonged presence of SRF.
Areas of hyperautofluorescence correspond to a long-standing accumulation of subretinal debris in cases of persistent SRF; in case of a re-attached retina, these areas may correspond to the location of SRF, as this may indicate a loss of photopigments.
Hypo-autofluorescent areas on FAF may correspond with the location of SRF accumulation (i.e., shadow artifacts) and/or RPE loss. In addition, granular hypo-autofluorescence on FAF may reflect RPE atrophy. With cCSC, the pattern of autofluorescence progresses relatively slowly, as it can take an average of 24 months for granular hypo-autofluorescent changes to progress to confluent hypo-autofluorescence. When an accumulation of debris from photoreceptor outer segments persists in the subretinal space—possibly after phagocytosis by macrophages—can appear as increased hyperautofluorescence.
Some patients with cCSC (and some patients with aCSC) who present with more marked and/or extensive atrophic changes in the RPE do not present with a dome-shaped PED, but present with a broader, shallow PED that may have an underlying neovascular component. A neovascular component should be considered when the space between the shallow PED—often referred to as FIPED (a flat, irregular PED) or SIRE (a shallow irregular RPE elevation)—and Bruch’s membrane on OCT contains mid-reflective material rather than being hyporeflective, which typically suggests SRF. In addition to these signs on OCT, en face swept-source OCT and OCT-A can be useful for detecting the presence of a secondary MNV—often a type 1 MNV—in combination with FA, and a subtle but visible well-demarcated neovascular structure on ICGA.
In a recent retrospective study involving 40 patients with cCSC who presented with evidence of a MNV in one eye, Mandadi et al. shown that one-fourth of the fellow eyes had a vascular network on OCT-A that was not readily detected on conventional imaging.
In severe cases of cCSC, a complication called posterior cystoid retinal degeneration (PCRD) can occur, in which cystoid fluid accumulates in the outer retinal layers. This accumulation of cystoid fluid does not always involve the central macula and is typically located extrafoveally, occurring at various locations in the posterior pole. These cystoid intraretinal spaces may be visible on OCT but unlike typical cystoid macular edema do not stain on FA. Thus, PCRD can contribute independently to the loss of central vision in patients with cCSC and is typically associated with long-standing cCSC. Cardillo Piccolino and colleagues studied 34 eyes with cCSC complicated by PCRD and found that BCVA ranged from 20/20 to 20/400, with BCVA 20/40 or better in eyes in which the intraretinal fluid spared the foveal center.
In a retrospective study, Sahoo and colleagues detected a MNV on OCT-A in 13 out of 29 cases of CSC with PCRD, but suggested that there may not be a direct correlation between the presence of MNV and PCRD.
Patients with cCSC often experience a gradual decline in both BCVA and contrast sensitivity due to damage to macular photoreceptors. In up to 13% of eyes with cCSC, this damage can lead to legal blindness, with BCVA reaching 20/200 or worse after 10 years. This decrease in BCVA can be due to changes in foveal atrophic RPE, photoreceptor damage, PCRD, and/or secondary MNV. Indeed, patients with cCSC report decreased vision-related quality of life, and a recent study involving 79 patients with aCSC or cCSC found that the decrease in vision-related quality of life was correlated with disease duration. Interestingly, however, 3 large RCTs found that at presentation vision-related quality of life scores among patients with cCSC were generally high, with mean scores of 81-88 on the 25-item National Eye Institute Visual Function Questionnaire.
Up to 42% of patients with cCSC present with signs of bilateral involvement on FA, even though most patients present with unilateral visual symptoms. Bilateral CSC is generally more common among patients over 50 years of age, with a prevalence of 50% in this age group compared to 28% of patients under the age of 50. Bilateral disease activity together with bilateral SRF is more common in severe cCSC phenotypes, present in up to 84% of cases. Moreover, patients with bilateral severe cCSC have a higher risk of developing severe, irreversible visual impairment. In some patients, CSC can present in one eye, with another disease in the pachychoroid spectrum presenting in the other eye.
Bullous CSC is a rare form of CSC often complicated by an exudative neuroretinal detachment with shifting SRF. In bullous CSC, multiple PEDs are often observed hidden beneath extensive SRF, and each PED can evolve into a RPE tear, after which an exudative retinal detachment may develop. Although severe forms of cCSC are typically progressive, the disease course can be slowed and in turn, BCVA stabilized or even improved with PDT treatment.
Finally, in cases of SRF with no clear signs of focal leakage, a wide range of diagnoses other than CSC should also be considered.
Optimizing the classification of CSC
CSC is commonly categorized as either aCSC or cCSC depending on the duration of the presence of SRF and atrophic RPE changes. However, CSC is a complex and variable disease entity that can present as several clinical subtypes; moreover, CSC can present as aCSC, but develop into cCSC over time. Thus, classifying CSC is extremely challenging. In addition, retina specialists often disagree when describing CSC cases. This high degree of discord among specialists was highlighted in a multicenter study by Singh et al., in which 6 retina specialists around the globe classified 100 cases of CSC using multimodal imaging data and relevant clinical details. These 6 specialists provided 36 different terms to classify the disease, with poor interobserver agreement. In addition, when the authors only considered the 3 most common descriptors—namely, “acute”, “chronic”, and “recurrent”—they found that the consistency was higher for diagnosing aCSC than for diagnosing either cCSC or recurrent CSC.
In response to the need for a revised CSC classification, the Central Serous Chorioretinopathy International Group recently proposed a new multimodal imaging-based classification system for CSC.
- This classification includes the following 2 major criteria, both of which must be met for a diagnosis of CSC:
- 1) the presence or evidence of a prior serous neuroretinal detachment documented on OCT involving the posterior pole, and unrelated to another disease process; and
- 2) at least one area of RPE alterations on FAF, spectral-domain OCT, or infrared imaging.
- In addition to these major criteria, at least one of the following criteria must be met in order to establish a diagnosis of CSC:
- 1) mid-phase hyperfluorescent placoid areas on ICGA;
- 2) one or more focal leaks on FA; and
- 3) SFCT ≥ 400 µm.
- Based on these criteria, the authors proposed classifying CSC as either simple or complex, with an area of RPE atrophy twice the size of the optic disc area serving as the threshold for differentiating between these classifications.
- In addition, they classified CSC cases with a bullous variant, cases with the presence of a RPE tear, and cases associated with another retinal disease as atypical.
- In addition to these major criteria, at least one of the following criteria must be met in order to establish a diagnosis of CSC:
The 2 main subtypes—simple CSC and complex CSC—were further subdivided into 3 groups, namely primary CSC (defined as the first known episode of SRF), recurrent CSC (defined as the presence of SRF with either a history or signs of resolved episodes), and resolved CSC (defined as the absence of SRF on OCT after a previous finding of SRF).
Changes in the outer retinal layer typically seen in long-lasting cases of CSC were also included in this classification system. Because the visual prognosis depends on involvement of the fovea, details regarding foveal involvement—whether in the form of serous neuroretinal detachment, outer retinal atrophy, or serous PED—were also included in the classification system. Lastly, the presence of a CSC-related MNV is also graded, as MNV is a distinct entity and is often associated with a poorer visual prognosis.
This novel classification has already been validated in several studies. For example, Chhablani and colleagues provided 10 masked retina specialists with clinical details and complete multimodal imaging data for 61 eyes in 34 patients with presumed CSC; these specialists then graded the cases using the above-mentioned classification system. They initially had moderate agreement, with kappa (κ) values of 0.57 (p < 0.0001) for the major criteria (after excluding a single outlier observer), and 0.58 for simple CSC, 0.62 for complex CSC, and 0.45 for no CSC. However, they had extremely poor agreement with respect to establishing a diagnosis of atypical CSC (κ = 0.008, p = 0.8). In a second round of grading, only the images of the fellow eyes were shown in order to determine whether the diagnosis of the affected eye might affect grading of the fellow eye. The authors found that when the grading was performed without prior information regarding the affected eye, the overall kappa value was significantly lower for all groups, and inter-grader agreement was also lower. This finding suggests that the type of CSC diagnosed in one eye is significantly influenced by the history and current state of the fellow eye; thus, disease grading should include both eyes at the same time, although specific grading can be performed separately for each eye. Similarly, Sahoo and colleagues asked 2 retina specialists to grade 87 eyes in 44 patients with previously undefined CSC. The authors found moderate to strong agreement between all subclassifications, including “simple or complex” (κ = 0.91, p < 0.001); “primary, recurrent, or resolved” (κ = 0.88, p < 0.001), and “foveal involvement” (κ = 0.89, p < 0.001). In addition, Arora and colleagues asked 2 masked retina specialists to grade multimodal imaging data from 93 patients with CSC and found near-perfect agreement (κ = 0.91; 95 % CI: 0.8–1.0) for the entire classification. Lastly, the same group performed a retrospective observational study involving 229 treatment-naïve eyes with CSC in which multimodal imaging data and clinical information were classified by 2 retina specialists using this new CSC classification. The authors found that both foveal involvement and the presence of outer retinal atrophy were associated with a lower BVCA. Despite these promising results, however, it should be noted that most of these studies included only 2 graders.
In conclusion, to date, this recently proposed classification system dividing CSC into simple versus complex disease is supported, albeit by a relatively small number of validation studies. These encouraging results require further validation—and possible refinement—of this new classification system. Moreover, how these grading systems correspond to patient outcome and/or the need for treatment remains an open question.
Risk factors for developing CSC
Several risk factors have been associated with CSC. First, studies have shown that men have a 2.7–8 times higher chance of developing CSC compared to women. In a recent study involving 1189 male androgen abusers and 11, 890 male controls, Subhi and colleagues found no correlation between androgen abuse and an increased risk of CSC, suggesting that biological male sex—and not simply androgen levels per se—may underlie the increased risk of CSC in men. A particularly high incidence of CSC has been reported in the age group of 35–44 years.
The use of corticosteroids is the most significant external risk factor for developing CSC, with odds ratios as high as 37:1 being reported, although lower odds ratios have also been described. Although rare, in some cases even minimal exposure to corticosteroids exposure (for example, inhalation, intranasal delivery, or intra-articular injection) has been associated with an increased risk, exacerbation, and/or recurrence of CSC, suggesting that the increased risk of developing CSC is not strictly dependent on the dose or mode of corticosteroid administration, but may also depend on genetic predisposition and/or an increased vulnerability to corticosteroid exposure in some individuals.
Interestingly, exhibiting type A behavioral characteristics (i.e., having an intense, sustained drive to achieve self-selected goals, an eagerness to compete, and a desire for recognition and advancement) has been suggested to be associated with CSC. In addition, a “CSC patient profile” has also been hypothesized to increase the risk of developing CSC, and this profile includes a drive to overachieve, impulsiveness, emotional instability, and a hard-driving sense of competitiveness. This notion may be plausible, as individuals who exhibit type A behaviors are believed to have increased levels of catecholamines and corticosteroids, which may underlie their apparent increased risk of developing CSC. Furthermore, stressful life events, engaging in shift work, poor sleep quality, and circadian rhythm disturbances have also been associated with a higher risk of CSC. In addition, several studies found an association between CSC and both certain personality traits and stress. On the other hand, a recent prospective study by Van Haalen and colleagues did not find an increased prevalence of cCSC among individuals with maladaptive personality traits such as type A behavioral characteristics compared to a reference group. However, this group did find that patients with cCSC used certain coping strategies (e.g., seeking social support, passive coping, and active coping in men) more than a reference group. Furthermore, studies have found that patients with CSC have more psychological problems, a lower quality of life, and higher levels of anxiety compared to healthy controls. Nevertheless, large, systematic studies that include detailed psychometric assessments such as suitable, validated questionnaires are needed in order to determine whether a genuine association exists between CSC risk and stress. To date, whether various techniques for reducing stress can have value in the treatment of CSC has not been fully investigated, and the use of extensive stress-reducing measures designed to curb CSC may not be recommended.
Cushing syndrome, a disorder in which the body produces excess levels of cortisol, has also been shown to serve as a risk factor for developing CSC. Interestingly, some studies found increased serum cortisol levels—although not high enough to establish a diagnosis of Cushing syndrome—in patients with CSC, whereas other studies did not find increased serum cortisol levels in patients with CSC. Moreover, CSC may be one of the presenting signs of Cushing disease. A prospective study by Brinks et al., which included 11 patients with active Cushing syndrome, found retinal abnormalities resembling subclinical CSC in 3 patients. In addition, a recent meta-analysis of macular exam performed in 189 eyes in 159 patients with Cushing syndrome and found CSC in 7.7 % of cases. Based on these findings, clinicians should consider referring patients with Cushing syndrome for an ophthalmological exam. Additional support for the putative link between CSC and Cushing syndrome comes from the report that SRF can resolve in patients following surgical treatment for Cushing syndrome, without the need to specifically treat the patient’s CSC. In another study involving 86 consecutive patients with cCSC, elevated 24 h urinary free cortisol levels were measured, suggesting increased activity of the hypothalamic-pituitary-adrenal axis; however, it is important to note that none of the patients with elevated cortisol levels met the clinical or biochemical criteria for Cushing syndrome. On the other hand, a subsequent study by the same group found that hair cortisol concentrations—a measure of longer-term cortisol levels—were similar between 48 patients with cCSC and 230 population-based controls, with no apparent correlation between hair cortisol concentration and cCSC severity.
Pregnancy has also been linked to a higher risk of developing CSC, possibly due to choroidal changes induced by abnormal hormone levels. For example, Kim et al. found no change in choroidal thickness in women who experience a normal pregnancy; in contrast, they found that pregnant women who develop preeclampsia showed hypertensive changes in the choroidal circulation, including choroidal hyperpermeability and stasis of choroidal vessels.
Another study of 9 women in China found that pregnancy-associated CSC developed predominantly in the third trimester and usually recovered spontaneously following delivery, with ultimately favorable BCVA; these results are consistent with a case report of pregnancy-related CSC. Given that pregnancy has been associated with an increased risk of CSC, women of childbearing age who present with CSC should be asked if they are or might be pregnant, and then monitored closely until delivery.
Additional risk factors for CSC have also been suggested and include gastroesophageal conditions such as Helicobacter pylori infection, uncontrolled systemic hypertension, use of antibiotics, allergy-based respiratory disease, high socioeconomic status, alcohol consumption, smoking, coronary heart disease, obstructive sleep apnea, poor sleep quality, shift work, autoimmune disease, short axial length, and hyperopia. In contrast, myopia has been associated with a lower risk of developing CSC. It should be noted, however, that these studies are not always consistent with respect to the putative link between these risk factors and CSC; therefore, larger and more rigorous studies are needed.
A familial predisposition to CSC has also been reported in several studies, suggesting that CSC may have a genetic component. Indeed, several single nucleotide polymorphisms (SNPs) have been associated with an increased CSC risk, some of which are located in genes involved in the complement system, including the CFH (complement factor H) and C4B (complement factor 4B) genes. Other genes associated with CSC include NR3C2 (encoding nuclear receptor subfamily 3 group C member 2, a mineralocorticoid receptor), ARMS2 (age-related macular degeneration susceptibility 2), CDH5 (cadherin 5), VIPR2 (vasoactive intestinal peptide receptor 2), SLC7A5 (solute carrier family 7 member 5), PTPRB (protein tyrosine phosphatase receptor type B), as well as the susceptibility loci rs13278062 at TNFRSF10A-LOC389641 and rs6061548 near GATA5 (GATA binding protein 5). A familial form of pachychoroid possibly inherited in an autosomal dominant pattern has also been reported by Lehmann and colleagues. Finally, genetic studies in Asian and Caucasian patients with CSC showed considerable overlap, specifically in the rs1329428 SNP in CFH, the rs13278062 locus at TNFRSF10A-LOC389641, and the rs6061548 locus near GATA5, indicating that CSC may have distinct, consistent genetic risk profile regardless of ethnicity.
Risk factors for disease recurrence and disease progression
If left untreated, approximately half (43–51 %) of patients with aCSC will develop at least one recurrence, while the 1-year recurrence rate after previous spontaneous resolution in cCSC is 30–52 %.
A number of risk factors have been associated with CSC recurrence and progression, including the use of corticosteroids, untreated hypertension, increased SFCT, non-intense hyperfluorescence on FA, shift work, male gender, older age, and sleep disorders. In addition, anxiety disorders and depression have also been suggested to increase the risk and/or recurrence of both aCSC and cCSC.
A study by Hosoda et al. showed that the CFH I62V genotype was predictive of spontaneous SRF resolution in patients with active CSC. Similarly, Kiraly et al. found that patients with CSC with the rs3753394 SNP in the CFH gene had an increased tendency for spontaneous SRF resolution at 3 months after disease onset. Moreover, both the CFH I62V and ARMS2 A69S genotypes were significantly associated with MNV development. A recent study by Yoneyama et al. found a significantly higher frequency of the CFH variants rs800292 and rs1329428 in patients with complex CSC (defined as the presence or absence of RPE alterations larger than 2-disc areas in either eye) compared to patients with simple CSC.
Moreover, Singh et al. found that a higher degree of damage in the ellipsoid zone (EZ) within the central 1000 μm of the fovea was associated with a decreased likelihood of SRF resolution. Lastly, the presence of a Fuji sign has also been associated with spontaneous SRF resolution.
However, all of the aforementioned studies regarding risk factors associated with disease recurrence and/or progression were relatively limited with respect to patient number and/or study design, and further studies are needed in order to confirm these putative associations.
Pathophysiology
Pachychoroid disease spectrum
The term pachychoroid literally means “thickened choroid” and was used in 2013 in a case series describing mild RPE alterations over areas of thickened choroid. This term is rather nonspecific, as no cut-off point for pachychoroid has been established and can depend on a number of additional factors such as age, axial length, refractive error, and the time of day at which choroid thickness is measured. In addition, variants in the CFH gene have associated with choroidal thickness among some Asian ethnic groups. Moreover, many patients who have a thickened choroid do not develop clinically relevant abnormalities or associated diseases considered part of the pachychoroid disease spectrum. In some rare cases, CSC can develop without the presence of pachychoroid. Although increased choroidal thickness is a major risk factor for CSC, choroidal dysfunction is another key factor that must be present in the pachychoroid disease spectrum; this is illustrated by the finding that although pachychoroid is usually associated with hyperopia, typical CSC can still develop in patients with emmetropic or myopic eyes combined with a choroidal thickness that falls within the normal range when refractive error is not considered.
The pachychoroid disease spectrum encompasses a number of clinical entities—including CSC—that have specific choroidal abnormalities in common. These clinical features—which can be appreciated on multimodal imaging—include a diffuse or focal increase in choroidal thickness, “pachyvessels” (dilated choroidal vessels in Haller’s layer) together with thinning of the inner choroid overlying these dilated vessels, and choroidal vascular hyperpermeability visible particularly on mid-phase ICGA. In addition to CSC, the pachychoroid disease spectrum also includes pachychoroid pigment epitheliopathy, peripapillary pachychoroid syndrome (peripapillary choroidal thickening associated with nasal macular intraretinal and/or subretinal fluid, as well as optic disc edema in some cases), pachychoroid neovasculopathy, and pachychoroid-associated polypoidal choroidal vasculopathy.
The pachychoroid disease hypothesis states that a sequence of events occurs wherein choriocapillaris hyperpermeability (including choroidal dysfunction) is followed by structural changes to the choriocapillaris, RPE complications, and—in some cases—neovascularization either with or without aneurysmal dilatations. However, many patients never progress to symptomatic advanced disease (e.g., extensive atrophic RPE changes, CSC, or neovascularization) with visual impairment. In uncomplicated cases of pachychoroid disease, isolated choroidal changes and thickening of the choroid without visible RPE and/or neuroretinal changes can occur. Although these patients do not yet present with RPE or and retinal abnormalities, ICGA may already show one or more mid-phase hyperfluorescent zones believed be typical of the pachychoroid disease spectrum. Over time, mild atrophic RPE changes can progressively appear; this manifestation is known as pachychoroid pigment epitheliopathy. As a disease in the pachychoroid disease spectrum, CSC is characterized by the presence of SRF leakage causing serous neuroretinal detachment. CSC is commonly associated with a variable degree of atrophic RPE abnormalities and is therefore often preceded by either symptomatic or asymptomatic pachychoroid pigment epitheliopathy, although patients with aCSC may also develop a single focal leak with no associated atrophic RPE changes. Individuals with uncomplicated pachychoroid, pachychoroid pigment epitheliopathy, or non-center-involving CSC are often asymptomatic. The last stage in the pachychoroid spectrum—pachychoroid neovasculopathy—is defined by the presence of a neovascular membrane, primarily in a shallow PED or FIPED as described in Section 1.1.2. Pachychoroid neovasculopathy can present with SRF either with or without a known history of CSC, and an associated component of polypoidal choroidal vasculopathy (PCV, also known as “aneurysmal type 1 neovascularization”) is not uncommon in these cases and may eventually develop with prolonged disease duration. Given the current ambiguity surrounding the term PCV, and to avoid confusion with neovascular AMD, Yamashiro et al. recently suggested using the terms “pachychoroid neovasculopathy without polypoidal lesions” and “pachychoroid neovasculopathy with polypoidal lesions”.
Whether the aforementioned diseases represent bona fide sequential stages in an underlying disease (i.e., “pachychoroid spectrum”) is currently unclear; however, several reports have documented the transition from one stage to the next. For example, pachychoroid pigment epitheliopathy has been shown to progress to more advanced stages, including CSC and PCV, and patients with CSC can also develop MNV and/or PCV.
Choroidal and scleral dysfunction in CSC
Back in 1967, Gass first suggested that hyperpermeability and increased hydrostatic pressure in the choroid can cause RPE damage, in turn leading to the development of a PED or SRF leakage through a defect in the RPE outer blood-retina barrier. Since then, multimodal imaging has shown typical choroidal abnormalities in patients with CSC. These abnormalities often include: one or more areas of focal indistinct hyperfluorescence on mid-phase ICGA, which reduces after PDT; increased choroidal thickness, which can decrease to normal values after PDT; dilated veins in Haller’s layer; an increased choroidal vascularity index (defined as the ratio between the luminal area and the total choroidal area); thinning of the choriocapillaris; and dysregulation of choroidal blood flow. The location of the SRF is often correlated with hyperfluorescent abnormalities seen on ICGA, which are believed to reflect vascular hyperpermeability of the choriocapillaris. Moreover, RPE alterations are believed to occur secondary to choroidal changes and dysfunction.
Recently, Spaide and colleagues proposed a novel theory to explain the pathophysiology underlying CSC, noting the important role of choroidal venous overload. Using imaging modalities such as ICGA and OCT to visualize the choroidal vasculature, this group and others found venous patterns in CSC eyes that are also seen in eyes following occlusion of the vortex veins and eyes with carotid cavernous fistulas. Eyes with CSC also exhibit choroidal abnormalities such as dilated veins, delayed choroidal filling, choroidal vascular hyperpermeability, imbalanced choroidal venous drainage, and intervortex venous anastomoses. Moreover, venous outflow abnormalities such as an abnormal Starling resistor effect appear to be intrinsic to CSC. Notably, arteriovenous anastomoses—direct connections between an artery and a vein that bypass the capillary bed—have also been suggested to play a role in the pathogenesis of CSC.
Studies suggest that congested choroidal outflow, vortex veins, and vascular resistance in CSC and other pachychoroid disease entities are associated with increased scleral rigidity and thickness.
Interestingly, Sawaguchi and colleagues recently found that the sclera was significantly thinner in eyes with steroid-induced CSC compared to eyes in patients with CSC who did not take steroids. Moreover, a recent report by Imanaga and colleagues showed that increased scleral thickness in CSC eyes is significantly correlated with increased choroidal luminal components, providing evidence to support the apparent close relationship between the choroid and sclera in CSC pathology. Furthermore, CSC eyes often present with loculation of fluid in the macula and peripheral ciliochoroidal effusion in association with increased scleral thickness.
Choroidal endothelial cells play an important role in regulating vascular permeability and vascular tone. The endothelium of the choriocapillaris is fenestrated, allowing for the diffusion of small molecules, as well as molecular exchange between the choroid and retina. Corticosteroids play a major role in the risk of developing CSC. Both the mineralocorticoid receptor (MR) and the glucocorticoid receptor (GR) have been suggested to have a pathogenic role in CSC. The glucocorticoid cortisol has variety of functional effects throughout the body, and cortisol levels increase in response to stress. Transcriptional changes induced by cortisol have been measured in endothelial cells in various tissues.
Interestingly, although GRs have been detected in choroidal endothelial cells, these cells do not appear to express presence of MRs. Consistent with this finding, the MR agonist eplerenone was not superior to placebo when tested as a possible treatment for cCSC in a large RCT.
On the other hand, several cortisol-regulated genes have been shown to play a role in endothelial cell function, including ZBTB16 (zinc finger and BTB domain containing 16), ANGPTL4 (angiopoietin-like 4), HIF3A (hypoxia-inducible factor 3 subunit alpha), SPARCL1 (SPARC Like 1), and PLAU (urokinase-type plasminogen activator). Specifically, cortisol has a marked effect on ZBTB16 expression, suggesting this gene may play an important role in the pathophysiology of CSC.
As discussed above, a variety of genes have been associated with an increased risk of CSC, including variants in CFH, C4B, ARMS2, CDH5, NR3C2, PTPRB, SLC7A5, TNFRSF10A, and VIPR2, some of which may be associated with choroidal endothelial cell function. A variant in the NR3C2 gene, which encodes the MR, increases the risk of CSC, thus providing a possible genetic basis to explain the putative link between corticosteroids and CSC. Moreover, variants in the CFH and VIPR2 genes have been associated with increased choroidal thickness. Further research is clearly needed in order to unravel the complex pathophysiology of CSC, particularly why men are considerably much more vulnerable than women.
Retinal pigment epithelium (RPE) dysfunction in CSC
Although RPE abnormalities are a clinical feature of CSC, the precise role of the RPE in the pathophysiology of CSC is poorly understood. Nevertheless, several hypotheses have been proposed to explain the role of RPE dysfunction in CSC. First, RPE dysfunction may trigger the accumulation of SRF and/or intraretinal fluid, and Negi and Marmor proposed that RPE defects might lead to an outflow of SRF from the choroid. Subsequently, Spitznas proposed an alternative theory in which a focal loss of RPE cell polarity induces the active transport of SRF to the subretinal space. However, a large body of evidence suggests that RPE defects occur secondary to choroidal dysfunction, and the choroidal abnormalities present in CSC are usually more extensive then the RPE abnormalities. Interestingly, the unaffected eye in patients with unilateral CSC can also present with RPE abnormalities, with typical underlying pachychoroid-associated choroidal hyperpermeability on ICGA, indicating that pachychoroid pigment epitheliopathy may in fact be a forme fruste of CSC, resulting from prolonged dysfunction.
RPE atrophy has been linked to reduced choroidal permeability, which shows as hypofluorescence on ICGA. This change in permeability may be due to progressive remodeling of the choriocapillaris after a long-lasting disease and chronic RPE atrophy, as the release of vascular endothelial growth factor (VEGF) from the RPE is needed to maintain the homeostasis and normal structure of the choriocapillaris. As a result, hydrostatic pressure from the choroid on the RPE may increase, eventually affecting RPE function and leading to an accumulation of SRF. Secondary damage to the RPE can range from small focal lesions to extensive degeneration, the latter of which has been described using the terms diffuse atrophic RPE alterations (DARA) and diffuse retinal pigment epitheliopathy (DRPE).
Lastly, as discussed above genome-wide association studies found that the rs13278062 SNP in the TNFRSF10A-LOC389641 locus is associated with both AMD and CSC. Interestingly, Mori et al. recently studied the functional role of TNFRSF10A in RPE degeneration using human primary RPE cells and Tnfrsf10 knockout mice. They found that TNFRSF10A was expressed in human RPE cells, and in vitro assays revealed that the rs13278062 SNP downregulates TNFRSF10A transcription in RPE cells, decreasing cell viability and increasing apoptosis by downregulating protein kinase C-alpha (PKC-α). Based on their findings, the authors suggested that downregulating TNFRSF10A expression inactivates PKC-α signaling and increases the vulnerability of RPE cells, thereby contributing to the pathogenesis of AMD and CSC.
Differential diagnosis
The differential diagnosis of serous maculopathy includes a broad range of diseases. As many as 13 distinct disease categories associated with—or mimicking—serous maculopathy were recently described by Van Dijk and Boon and include: ocular neovascular diseases, vitelliform lesions, inflammatory diseases, ocular tumors, hematological malignancies, paraneoplastic syndromes, inherited retinal dystrophies, ocular development anomalies, medication-related conditions and toxicity-related disease, rhegmatogenous retinal detachment and tractional retinal detachment, retinal vascular disease, as well as a miscellaneous category that includes serous maculopathy secondary to RPE dysfunction due to confluent drusen, serous maculopathy with absence of RPE (SMARPE), serous maculopathy due to aspecific choroidopathy (also described as stellate macular choroidopathy, or SMACH).
Distinguishing between these diseases requires multimodal imaging, often including OCT, OCT-A, FA, FAF, and/or ICGA. In addition to the clinical characteristics such as male preponderance and an age at onset of 20–55 years, several key findings on imaging help differentiate between CSC and other diseases. These findings include: one or more PEDs on OCT; increased choroidal thickness with dilated vessels in Haller’s layer (pachyvessels) often associated with a thinned overlying choriocapillaris and RPE changes; focal or multifocal leakage on FA; and—perhaps one of the most typical signs of CSC or pachychoroid disease spectrum—one or more areas of indistinct hyperfluorescence in the affected eye—and often the fellow eye as well—on mid-phase ICGA.
Treatment for CSC
Determining the optimal treatment for CSC can be challenging due to the wide variety in disease presentation and clinical course, the current lack of consensus regarding a classification system, and the disease’s poorly understood pathophysiology. Moreover, some treatment options—particularly PDT—are not available in all countries, and some of treatments may not be covered by the patient’s health insurance. The ideal treatment should have a favorable safety profile, particularly given that CSC has a relatively good visual prognosis, even if left untreated in many cases. Importantly, the inclusion and exclusion criteria, study endpoints, and clinical definitions vary among retrospective studies regarding the treatment of CSC. The relatively high rate of spontaneous SRF resolution in aCSC—and in up to 30 % of cCSC cases—may explain the apparent promising results reported for a range of treatments studied in non-systematic, non-prospective, non-randomized studies, but these results have not been replicated by sufficiently powered prospective RCTs. If a study is not properly designed—for example, by lacking a suitable control group—the researchers may reach the potentially false conclusion that the treatment was effective, particularly if they fail to take into account spontaneous improvement. However, 3 large investigator-initiated multicenter RCTs for the treatment of cCSC were recently published. These studies and a number of other RCTs helped to establish an evidence-based treatment guideline for CSC based on currently available data.
Aims of treatment
The ultimate goal in treating CSC is to achieve complete SRF resolution, thereby preserving the outer neurosensory retinal layers, as even a small amount of persistent SRF can lead to irreversible damage. To restore the normal photoreceptor-RPE interaction, complete SRF resolution should therefore be one of the primary endpoints in intervention trials regarding the treatment of CSC. Patients with CSC often have a gradual improvement in visual symptoms and visual function after the photoreceptor-RPE interaction is restored. However, even after successful treatment (i.e., complete resolution of SRF), visual symptoms can persist due to preexisting irreversible neurosensory retinal and/or RPE damage, and these symptoms can include suboptimal BCVA, loss of contrast and/or color vision, and metamorphopsia. Nevertheless, an intriguing question is why the visual prognosis is generally much better with subfoveal SRF associated with CSC compared to subfoveal SRF associated with a rhegmatogenous retinal detachment.
In addition to complete SRF resolution, another important goal in the treatment of CSC is to preventing recurrence and future disease progression.
Elimination of risk factors
In addition to actively treating CSC, eliminating potential risk factors can play an important role in improving the treatment of CSC, regardless of the subtype of CSC. For instance, patients with CSC should be advised to discontinue the use of all forms of corticosteroids, provided that this is clinically feasible. Patients who present with one or more symptoms suggestive of Cushing disease such as abdominal obesity, abdominal stretch marks, muscle weakness, easy bruising, facial rounding and flushing, osteoporosis, hypertension, diabetes mellitus, the presence of dorsal fat pads, and/or neuropsychiatric symptoms should be referred to an endocrinologist. Notably, ophthalmologists should be aware that in some patients CSC can serve as the primary presenting feature of Cushing disease, as the symptoms listed above can be very subtle.
Treatment options for CSC
Photodynamic therapy (PDT)
Although PDT was originally developed as a treatment for skin cancer, it has now used in ophthalmology for over 2 decades. For example, the light-sensitive compound verteporfin is approved for use in PDT for the treatment of MNV caused by either AMD or pathological myopia. Verteporfin has also been used as an off-label treatment for CSC, particularly cCSC.
Verteporfin binds to plasma low-density lipoproteins, which then bind to surface receptors on vascular and reticuloendothelial cells. The therapeutic effect of PDT is believed to be based on the release of free radicals when the treatment site is illuminated in association with the photosensitizing dye, and this effect is primarily activated in the choriocapillaris. This may then be followed by remodeling of vessels in the capillary bed in the vascular endothelium. Because of the high selectivity of verteporfin for choroidal blood vessels, retinal photoreceptors are not affected by PDT, and the risk of damage to the RPE is also low. PDT for the treatment of CSC has been extensively studied since the first report of its use in this condition.
Treatment algorithms and mode of action. In the first studies evaluating the potential of using PDT as a treatment for CSC, either “standard” or “full” settings—similar to the settings typically used for the treatment of neovascular AMD—were used. The standard settings include a verteporfin dose of 6 mg/m2, 689-nm wavelength laser light delivered at 50 J/cm2 fluence at an intensity of 600 mW/cm2, and a treatment time of 83 s. To avoid the potential though rare complication of profound ischemia in the choroid—as observed on a few occasions following PDT for neovascular AMD—several alternative PDT regimens have been described using reduced treatment settings such as reducing the verteporfin dose by half (3 mg/m2 instead of 6 mg/m2), using half fluence (25 J/cm2 instead of 50 J/cm2), and/or half of the original treatment time (42 s instead of 83 s).
Before performing PDT, the target area to be irradiated with a circular spot of light must be properly selected. The target area is often set so that the diameter of this spot covers the hyperfluorescent area(s) on mid-phase ICGA and the corresponding point(s) of leakage on FA and OCT. Currently, ICGA-guided PDT is more common than FA-guided PDT, which used to be the standard. Using ICGA to target the choroidal abnormalities with the PDT laser spot can help ensure that the underlying choroidal abnormalities are treated with maximum efficacy. The macula should be treated first, immediately followed by additional treatment spots, if needed.
Whether several spots can overlap during the treatment regimen is an open question.
Prior to PDT, the pupil should be dilated using a topical mydriatic agent, followed by either 6 mg/m2 (full-dose) or 3 mg/m2 (half-dose) verteporfin delivered via an intravenous infusion over a period of 10 min. An anesthetic eye drop (e.g., oxybuprocaine 0.4 %) is then administered, a contact lens (typically a 1.6× magnification PDT lens) is positioned on the eye, and treatment is performed with 15 min after the start of verteporfin infusion. For full-fluence PDT, light at 689 nm with a fluence of 50 J/cm2 is applied for 83 s to the designated area. In the case of half-fluence PDT in combination with full-dose verteporfin (6 mg/m2), a fluence of 25 J/cm2 for 83 s is used. Lastly, half-time PDT may also be used, which includes full-dose verteporfin (6 mg/m2), full-fluence (50 J/cm2), for a treatment time of 42 s. After treatment, patients should be advised to avoid exposure to direct sunlight and other sources of UV radiation (particularly 689-nm wavelength light), as patients remain photosensitive for up 48 h after treatment, even with half-dose PDT.
Importantly, half-dose PDT has been shown to be equally effective as—or even superior to—full-dose, half-fluence, and half-time PDT regimens for the treatment of both aCSC and cCSC.
Half-dose PDT may be preferred over half-fluence and half-time PDT, for several reasons. First, more prospective and sufficiently powered retrospective data support the efficacy of half-dose PDT compared to other treatment regimens. Second, half-dose PDT may have a reduced risk of photosensitivity due to the lower dose of systemic verteporfin. Finally, using half the verteporfin dose per patient means that a single-dose vial of verteporfin can be used to treat 2 patients, which reduces treatment cost and can increase verteporfin availability in times of shortage; however, in some countries such as the US, using 1 vial to treat 2 patients can be problematic and can have legal consequences with respect to insurance billing.
Choroidal thickness may temporarily increase following half-dose PDT for CSC, and this transient choroidal thickening can be accompanied by a temporary increase in SRF, with worsening of visual symptoms lasting up to 4 weeks reported in up to 38 % of PDT-treated patients. These treatment-related changes generally improve within 1–3 weeks after PDT, with gradual improvements in anatomical and functional outcome. In patients with unilateral CSC, choroidal thickness in the treated (i.e., affected) eye can decrease to the same thickness as the fellow (i.e., unaffected) eye, suggesting that PDT can reduce choroidal thickness to relatively normal levels. In addition, PDT has been shown reduce choroidal hyperpermeability and leakage on ICGA.
Studies regarding PDT for the treatment of CSC often include more patients with cCSC and fewer patients with aCSC, as spontaneous resolution is more common in aCSC. Two studies found no significant difference between half-fluence PDT and half-dose PDT with respect to outcome for the treatment of cCSC, although another study found that half-dose PDT led to earlier complete SRF resolution compared to half-fluence PDT measured at the 1-month follow-up visit. In a retrospective study, Park et al. compared full-dose, half-dose, and half-dose/half-fluence PDT and found that both full-dose and half-dose PDT were effective in terms of significantly improving BCVA, whereas the half-dose/half-fluence PDT had no significant effect. Other studies found similar efficacy between half-fluence PDT and full-fluence PDT for the treatment of cCSC, although a retrospective study by Son et al. found that patients treated with full-fluence PDT had an overall larger reduction in SFCT compared to patients treated with half-fluence PDT. In addition, 2 studies showed similar results between half-time PDT and half-dose PDT. Furthermore, a previous study by Liu et al. found that patients with cCSC who were treated with half-dose/full-fluence PDT had a higher rate of complete SRF resolution compared to patients treated with half-dose/half-fluence PDT.
Several studies also compared various dosages of verteporfin in an attempt to determine the lowest effective treatment dosage for CSC. Specifically, one-third dosage was compared to half-dose PDT and was found to be inferior primarily in terms of SRF recurrence rate and improvement in BCVA.
PDT in acute CSC. Although spontaneous SRF resolution is relatively common in aCSC, treatment of aCSC with PDT has been studied in a few RCTs, with complete SRF resolution reported in 74–100 % of cases. First, Chan et al. performed a prospective, placebo-controlled, RCT involving 63 patients with aCSC; 43 patients were randomized to receive ICGA-guided half-dose PDT, and 21 patients received placebo. The authors found that complete SRF resolution at 12 months was achieved in 95 % of patients who received half-dose PDT compared to only 58 % of patients who received placebo, a significant difference between groups. Moreover, mean BCVA at 12 months was significantly better in the treatment group compared to the placebo group. These results suggest that half-dose PDT may be a viable treatment option for aCSC, despite the high probability of achieving spontaneous SRF resolution if left untreated.
In contrast, Missotten and colleagues performed a RCT to assess whether PDT can be safely deferred in aCSC when the leakage point on FA is within 1 optic disc diameter from the fovea. This study included 52 patients; half randomized to receive half-fluence PDT and evaluated at 3 months (with subsequent follow-up visits every 3 months), while the other 26 patients were randomized to observation only. At 3 months, BCVA improved faster and metamorphopsia improved significantly in the PDT group compared to the control group, although no statistically significant difference was observed between the 2 groups at 12 months. It should be noted that PDT was performed if any leakage or SRF was observed at the 3-, 6-, or 12-month evaluation visit, regardless of the group, which may have obscured the results at the 12-month follow-up visit, particularly given the relatively low number of patients in each group.
Some retrospective studies of patients with aCSC have found that PDT can provide faster SRF resolution and a more rapid recovery of retinal sensitivity, and additionally, a higher BCVA improvement compared to placebo was observed in a RCT. Two RCTs compared PDT settings for the treatment of aCSC. The first study, by Zhao and colleagues, found that half-dose PDT (i.e., 50 % of the standard dose) was more effective at inducing complete SRF resolution and achieving better visual outcome than 30 % of the standard dose. More recently, Hu et al. studied 51 eyes in 45 patients with aCSC and found that SRF resolved completely in 57 % and 91 % of eyes 1 month and 3 months, respectively, in patients who received ICGA-guided half-dose PDT, compared to 70 % and 96 %, respectively in patients who received OCT-A‒guided half-dose PDT. Thus, OCT-A‒guided PDT was noninferior to ICGA-guided PDT with respect to complete SRF resolution at 3 months.
In addition to the aforementioned RCTs in aCSC, which had relatively small sample sizes, a number of non-randomized retrospective studies regarding the use of PDT in the treatment of aCSC have also been performed. For example, Kim et al. compared outcome in 11 patients who received FA-guided half-dose PDT and 10 patients who received placebo. The authors found complete SRF resolution in 80 %, 100 %, and 90 % at 1, 3, and 12 months, respectively, in the PDT groups, compared to only 18 %, 27 %, and 64 % of patients, respectively, in the placebo group. Additionally, the long-term change in BCVA and the rate of complete SRF resolution were not significantly different between patients who received half-dose PDT compared to patients who did not receive any treatment (with 90 % and 64 % of patients, respectively, achieving complete SRF resolution at 12 months).
Treatment with low-fluence PDT may also lower the risk of SRF recurrence in aCSC. For example, Ozkaya et al. performed a case-control study involving 77 patients and found that 51 % of untreated patients had a recurrence of SRF, compared to only 25 % of patients treated with low-fluence PDT. In addition, Mohabati and colleagues performed a large retrospective study including 295 eyes with typical aCSC (which the authors defined as documented presence of SRF on OCT, only one area of focal leakage on FA, and limited RPE alterations—including PEDs—of an area smaller than 1 optic disc) and found that SRF recurrence occurred in 24 % of untreated eyes, compared to only 4 % of eyes that received early treatment, the majority of which received half-dose PDT.
In conclusion, even though patients with aCSC have a relatively high likelihood of spontaneous SRF resolution, half-dose PDT seems to be a suitable treatment option for aCSC, as it may lead to more rapid SRF resolution and more rapid recovery of retinal sensitivity, and may therefore be indicated for some patients, particularly those who require a rapid improvement in vision, for example for professional reasons. On the other hand, simply observing patients with aCSC for several months does not seem to significantly affect long-term visual outcome.
PDT in chronic CSC. PDT as a treatment for cCSC was first reported by Yannuzzi and colleagues in 2003, in which the authors reported complete SRF resolution in 12 out of 20 eyes (60 %) at 6 weeks following PDT using standard (“full dose”) settings. In the same year, Cardillo Piccolino et al. reported complete SRF resolution in 12 out of 16 eyes (75 %) at 1 month following full-dose PDT. Although short-term and long-term adverse effects of full-settings PDT in cCSC are extremely rare, several subsequent studies used a reduced verteporfin dose for the treatment of cCSC, providing evidence of a better safety profile and similar efficacy compared to full-dose PDT, half-fluence PDT, and half-time PDT.
In recent years, several RCTs have added to the body of evidence supporting the use of half-dose PDT as a first-line treatment for cCSC. First, the investigator-initiated PLACE trial by Van Dijk et al. and the first large RCT in cCSC compared ICGA-guided half-dose PDT to high-density subthreshold micropulse laser treatment (HSML) in 179 patients with cCSC. At 6–8 weeks following treatment, SRF had resolved in 51 % of the half-dose PDT‒treated patients, compared to only 14 % of the HSML-treated patients (p < 0.001). A similar improvement in the PDT group was also observed at 7–8 months, with 67 % and 29 % of patients, respectively, having resolved SRF (p < 0.001). In addition, 6–8 weeks after treatment, the PDT-treated patients had a significantly higher increase in BCVA compared to the HSML-treated patients (+4.60 ETDRS letters vs. +1.39 ETDRS letters, respectively, p = 0.011), although this difference was no longer significant 7–8 months after treatment (+6.78 and + 4.48 ETDRS letters, respectively, p = 0.099).
Retinal sensitivity on microperimetry has also been shown to be an important measure of successful treatment, as BCVA can be relatively preserved in patients with CSC, despite the presence of SRF.
In the PLACE trial, the increase in mean retinal sensitivity was significantly higher at both 6–8 weeks (p = 0.046) and 7–8 months (p = 0.008) in the half-dose PDT group than in the HSML group.
The patients with cCSC who presented with persistent SRF at their final visit during the PLACE trial despite receiving the primary treatment (half-dose PDT or HSML) were subsequently invited to participated in a follow-up crossover study—the REPLACE trial—and received the crossover treatment (i.e., those who received half-dose PDT in the PLACE trial received HSML in the REPLACE trial, and vice versa). In this crossover study, 82 % of the 32 patients who received half-dose PDT as the crossover treatment had complete SRF resolution 6–8 weeks after treatment, compared to 0 % of the 10 patients who received HSML patients; moreover, increase in mean retinal sensitivity was significantly larger in the PDT group compared to the HSML group (p < 0.001).
- In a second follow-up study of the PLACE trial, 44 patients with cCSC (specifically, 29 and 15 patients, respectively, who had received half-dose PDT and HSML, respectively, in the PLACE trial) who had achieved complete SRF resolution at the end of the PLACE trial were evaluated one year later. These authors found that 93 % of the patients in the half-dose PDT group still had complete SRF remission at their 1-year visit, compared to only 53 % of patients in the HSML group (p = 0.006), indicating that patients with cCSC who receive ICGA-guided HSML are less likely to achieve long-term SRF remission. The authors suggested that this finding may be due to the fact that unlike PDT, HSML does not target the choroid, the tissue primarily affected in CSC. In addition, patients who were successfully treated with half-dose PDT in the PLACE trial (defined as complete SRF resolution at the final visit) were also less likely to have SRF recurrence at 20 months compared to patients successfully treated with HSML. However, the authors found no difference in functional outcome between these 2 treatment groups at the long-term follow-up.
A subsequent investigator-initiated RCT in the Netherlands called the SPECTRA trial compared treatment with half-dose PDT to treatment with oral eplerenone (25 mg/day for 1 week, then increased to 50 mg/day if the patient’s potassium levels were sufficient) in 107 patients with cCSC. Three months after baseline, significantly more patients in the half-dose PDT group had complete SRF resolution compared to the eplerenone-treated patients (78 % vs. 17 %, respectively, p < 0.001), as well as a significantly larger increase in retinal sensitivity (p = 0.041). Similar to the findings reported in the REPLACE trial, the patients in the SPECTRA trial who had persistent SRF 3 months after primary treatment then received the crossover treatment and were evaluated 3 months later in the follow-up SPECS trial. Three months after crossover treatment, 32 out of 37 (87 %) of patients who received half-dose PDT as the crossover treatment still had complete SRF resolution, compared to only 2 out of 9 patients (22 %) who received eplerenone as the crossover treatment (p = 0.030). Furthermore, the patients who were enrolled in the SPECTRA trial were re-evaluated 12 months after baseline, with complete SRF resolution observed in 90 % and 88 % of patients who were initially received half-dose PDT or eplerenone, respectively. This small difference between treatment groups should be taken with a grain of salt, however, as 83 % of the 42 patients who initially received eplerenone subsequently received half-dose PDT in the SPECS crossover trial due to persistent SRF on OCT, compared to only 22 % of the patients initially received half-dose PDT followed by eplerenone treatment in the SPECS trial. Nevertheless, the 12-month improvement in BCVA was significantly larger in the patients who initially received primary half-dose PDT compared to the patients who initially received eplerenone (p = 0.030), despite no significant difference in macular retinal or foveal sensitivity on microperimetry measured between these 2 groups at the 1-year follow-up visit.
Lastly, Park and colleagues performed a RCT involving 43 eyes in 42 patients with cCSC in order to investigate the effect of using different fluence rates (50 %, 40 %, and 30 %) with PDT. The authors found that a 50 %-fluence was the most effective, with the lowest recurrence rate (0 %) and the highest rate of complete SRF resolution (100 %) at 12 months, compared to recurrence rates of 46 % and 25 % in the 40 %-fluence and 30 %-fluence groups, respectively, and complete SRF resolution rates of 60 % and 81 %, respectively. In addition, 12 months after PDT, mean BCVA improved significantly in both the 50 %-fluence (p = 0.003) and 40 %-fluence (p = 0.005) groups relative to baseline, but not in the 30 %-fluence group.
Several retrospective studies using PDT for the treatment of cCSC have also been performed, with complete SRF resolution rates ranging from 21 % to 100 %. For example, in a large retrospective study of 204 patients with cCSC Fujita et al. found complete SRF resolution in 89 % of patients 12 months after half-dose PDT. Moreover, the long-term benefits of half-dose PDT are generally favorable, as 2 studies found complete SRF resolution rates of 81 % and 91 % after a mean follow-up of 50 and 19 months, respectively. Reduced-settings PDT also has favorable long-term outcome with respect to BCVA, with an average increase of 5 ETDRS letters measured 7–8 months after reducing-settings PDT in the PLACE trial, and a mean increase of 9 ETDRS letters in patients 4 years after receiving full-settings PDT.
Recurrence of SRF after prior complete resolution was also examined after ICGA-guided half-dose PDT for cCSC. Dhirani and colleagues found that SRF recurred in 13 % of patients after a mean follow-up of 19 months, Haga et al. found a recurrence rate of 18 % after a mean follow-up of 50 months, while Son et al. found a recurrence rate of 0 % after a mean follow-up of 40 months. In a retrospective study of 61 patients who underwent half-time PDT, Hayashisa et al. found that patients who underwent FA-guided half-time PDT had a significantly higher rate of recurrence and/or persistent SRF compared to patients who underwent ICGA-guided half-time PDT. This difference in efficacy between FA-guided and ICGA-guided PDT may be explained by the fact that choroidal abnormalities are the underlying cause of CSC; thus, FA-guided PDT may not sufficiently treat CSC, as abnormalities identified on FA are generally more focal than—and secondary to—the underlying choroidal abnormalities.
In the treatment of cCSC, half-dose PDT has been associated with a lower recurrence rate compared to PDT using lower doses. Moreover, Silva and colleagues found that only 3 out of 46 (4 %) eyes with cCSC had persistent SRF 4 years after receiving full-dose PDT. In addition, the likelihood of SRF recurrence is lower after PDT compared to both HSML and oral eplerenone. One year after treatment in the PLACE trial, only 7 % of patients who received half-dose PDT had a recurrence of SRF, compared to nearly half (47 %) of the patients who received HSML. In a retrospective study of 75 eyes with unspecified CSC treated with either half-dose PDT or placebo, by Lai and colleagues found that only 20 % of eyes in the half-dose PDT group had a recurrence of SRF compared to 53 % of eyes in the placebo group at the 3-year follow-up visit. In a subsequent study, Lai et al. found that compared to patients with unilateral cCSC the recurrence rate after half-dose PDT was higher in patients with bilateral cCSC, possibly indicating more severe and/or extensive disease.
Several predictors of treatment outcome following PDT for CSC have been reported, including: 1) the presence of posterior cystoid retinal degeneration; 2) absence of an intense hyperfluorescent area on ICGA prior to PDT; 3) poor baseline BCVA; 4) a disruption in the EZ; 5) a diffuse (i.e., not focal) hyperfluorescent pattern on ICGA; 6) the presence of shallow, irregular PEDs on OCT, which can be suggestive of type 1 MNV; and 7) lower central macular thickness at baseline. Interestingly, a study by Breukink et al. did not find a clear correlation between corticosteroid use and outcome after PDT in patients with cCSC. Importantly, if the disruption in the EZ remains after complete SRF resolution, BCVA can remain poor.
In some cCSC cases, re-treatment with PDT may be required due to persistent SRF. However, in the PLACE trial, only 32 % of patients who received a second round of half-dose PDT due to persistent SRF achieved complete SRF resolution at their subsequent follow-up visit. Importantly, hypofluorescent changes on ICGA may predict a potential lack of response to repeated PDT. RPE atrophy has been linked to reduced choroidal permeability, which results in hypofluorescence on ICGA, possibly due to progressive quiescence of the choriocapillaris after long-lasting disease and chronic RPE atrophy. If choroidal leakage and congestion are present—which can be seen as multifocal hyperfluorescence on ICGA and multifocal leakage on FA—the patient is more likely to have a favorable response to PDT than if the choriocapillaris is thinned and quiescent due to chronic damage. Nevertheless, a second PDT treatment may still be effective in some patients with CSC, particularly cases with SRF due to persistent—or recurrent—hyperfluorescent choroidal changes on ICGA in association with focal leakage on FA.
Several studies have also examined PDT for the treatment of PEDs associated with SRF in CSC and found positive results regarding complete PED resolution. For example, a retrospective study of 123 patients with macular PED who were treated with either half-dose PDT or HSML in the PLACE trial found that half-dose PDT was significantly better than HSML with respect to reducing the height of macular PEDs in active cCSC. In a retrospective interventional study, 35 eyes in 35 patients with serous subfoveal PED associated with CSC were treated with reduced-fluence PDT (with 6 mg/m2 verteporfin and 30–36 mJ/cm2 light intensity); 1 month after treatment, 28 eyes (80 %) had complete resolution of the subfoveal PED, and recurrences of subfoveal PEDs were observed 10 months after treatment.
In conclusion, a growing body of evidence obtained in recent years support the use of half-dose PDT as the preferred treatment option for cCSC. Nevertheless, a large RCT comparing half-dose PDT to placebo is warranted in order to further demonstrate the efficacy of half-dose PDT.
Safety of PDT in CSC. An initial concern regarding the safety of PDT in CSC was the risk of choroidal ischemia and subsequent retinal atrophy, based primarily on previous reports of choroidal ischemia and vision loss in patients with AMD treated—often multiple times—with PDT using standard (“full”) settings. However, extrapolating data from AMD to CSC can be difficult given the differences in their etiology and age of onset. In AMD, the choroid is generally reduced at baseline and presents with an altered RPE and often the presence of sub-RPE material such as drusen. This constellation of findings is in stark contrast with CSC and the pachychoroid disease spectrum, which typically present with an abnormally thickened choroid, dilatation and overload of the veins in Haller’s layer, and a dysfunctional, hyperpermeable choriocapillaris. In CSC, PDT—applied using either standard or reduced settings—actually reverses the abnormally thickened choroid and reduces choroidal hyperpermeability; in contrast, PDT in both AMD and PCV is aimed at the retinal and/or subretinal neovascularization. This difference likely underlies the findings PDT-induced choroidal ischemia and acute vision loss is extremely rare in CSC cases.
Importantly, several large prospective RCTs and many retrospective studies have shown that adverse events are rare following half-dose PDT. Importantly, using higher laser fluence or a higher dosage of verteporfin may increase the risk of adverse events. For example, Schlotzer-Schrehardt and colleagues found that both the risk and severity of adverse effects increased when fluence was 100 J/cm2, double the standard fluence of 50 J/cm2 and 4 times the fluence used in half-fluence PDT, which is often used for the treatment of diseases in the pachychoroid disease spectrum. In addition, a meta-analysis comparing full-dose PDT to placebo in patients with MNV due to AMD, a higher prevalence of visual disturbances were reported in the PDT-treated group compared to the placebo group (22–42 % versus 16–23 %, respectively), including visual field defects and decreased and/or abnormal vision. In addition, the authors found that 1–5 % of the patients treated with full-dose PDT experienced an acute decrease in BCVA; however, Arnold et al. found that up to 71 % of patients with AMD who experience an acute decrease in BCVA improved by at least one line after 3 months. On the other hand, a study involving 46 cCSC eyes in 42 cCSC found that full-dose PDT was not associated with either systemic or ocular side effects up to 4 years after treatment.
Adverse events associated with PDT can include systemic events such as headache, back pain, nausea, dyspnea, dizziness, and syncope. These adverse events can present after both full-settings and reduced-settings PDT and are related to the use of verteporfin. Side effects at the site of verteporfin infusion can also occur and can include skin edema, pain, extravasation, and inflammation; however, these side effects are relatively rare, occurring in <1 % of cases. In addition to systemic side effects related to verteporfin infusion, other—albeit extremely rare—side effects can include a hypersensitive reaction to the infusion (including an anaphylactic reaction with convulsions) and temporary renal artery stenosis, which can manifest as severe back pain during verteporfin infusion and typically resolves after stopping the infusion. Pregnancy, porphyria, and poor liver function are contraindications for PDT.
Although uncommon, ophthalmic adverse events have also been reported to occur following half-dose PDT. One such short-term adverse event, PDT-induced acute exudative maculopathy (PAEM), was recently identified. PAEM is defined as subretinal exudation occurring within days following PDT and can present either with or without an acute decrease in vision. Thus, although difficult to confirm transient choroidal ischemia and inflammation, which can result in excessive vascular permeability, may underlie this adverse event. Recently, Fernandez-Vigo and colleagues performed a prospective observational case series involving 92 eyes in 75 patients with CSC in which SRF was present for at least 3 months and who underwent half-fluence PDT during which the treatment spot was centered on the fovea. The authors found that PAEM occurred 3 days after PDT in 28 out of 92 eyes (30.4 %), although they found no significant difference in the rate of complete SRF resolution at 3 months between patients who developed PAEM and patients who did not. Interestingly, on average the patients who developed PAEM had a worse baseline BCVA compared to patients who did not develop PAEM (72 vs. 77 ETDRS letters, respectively, p = 0.048). The authors performed a long term-follow up study, which included 64 eyes of 64 of the aforementioned patients who had a follow-up of at least 2 years. At 2 years, there were no differences in BCVA change between patients with and without PAEM, with an increase of 4.2 and 7.1 ETDRS letters, respectively (p = 0.055). In addition, a small prospective study by Van Dijk et al. involving 14 eyes in 13 patients with cCSC who underwent half-dose PDT found worsening of visual complaints in 5 patients (38 %) 1 week after treatment, with no significant difference in central foveal thickness, SRF height, choroidal thickness, or retinal sensitivity on microperimetry between in the 5 patients who experienced worsening of visual symptoms and the 8 patients who did not. In summary, although acute post-PDT PAEM is not particularly uncommon, it appears to have a self-limiting course and favorable outcome.
Previously, Yannuzzi suggested that baseline presence of subretinal fibrin in the serous detachment in CSC—which may be associated with lower baseline BCVA and poorer outcome if left untreated—may be a risk factor for vision loss following PDT. However, Liang et al. conducted a relatively large case series in patients with unspecified CSC who received half-dose PDT and found no difference in BCVA improvement or SRF resolution between patients who presented with subretinal fibrin and patients who presented without subretinal fibrin; moreover 91.7 % of patients with subretinal fibrin at baseline achieved complete SRF resolution and good visual outcome, with no ocular adverse events reported.
Long-term ophthalmic adverse events following PDT are relatively rare, but can include atrophy of the RPE, atrophy of the choroid, and development of a MNV; however, all of these events can also occur naturally, making a causal link between these complications and PDT difficult to establish. Despite the favorable safety profile of PDT for the treatment of CSC, a retrospective study by Lim and colleagues revealed RPE atrophy and an acute severe decrease in vision in 4 % and 1.5 % of eyes, respectively, in patients with unspecified CSC who received either half-fluence PDT (128 patients) or full-fluence PDT (130 patients). On the other hand, we recently studied 57 patients with cCSC from the PLACE and SPECTRA RCTs who were treated with fovea-involving half-dose PDT, but found no signs of RPE atrophy on multimodal imaging 2 years after treatment. Another recent study by Pinto et al. found that similar efficacy and safety following foveal and extrafoveal application of half-dose PDT in 70 eyes in 47 patients with cCSC.
In a recent retrospective interventional study involving 559 eyes in 520 patients with CSC who received PDT, Hwang et al. found that 1.25 % of eyes developed MNV within 3 months; specifically, 6 out of 138 eyes (4.35 %) with a flat irregular PED developed MNV, compared to only 1 out of 421 eyes (0.24 %) without a flat irregular PED (p < 0.001). In addition, a retrospective interventional case series that included 204 eyes with cCSC treated with half-dose PDT found no ocular or systemic side effects other than a polypoidal lesion in one patient 8 months after treatment. However, it should be noted that the development of PCV can reflect the natural course of CSC, as the presence of MNV is relatively common, with reported rates as high as 36 % among patients with cCSC prior to receiving treatment; thus, the development of MNV may not necessarily be attributed solely to PDT. In addition, a retrospective study by Shin et al. found no difference in MNV development between patients with CSC were treated with a focal laser (1 out of 33 eyes developed MNV after 12 months) compared to patients treated with half-dose PDT (1 out of 29 eyes developed MNV after 81 months). Lastly, Wu and colleagues studied 70 eyes in 61 patients with cCSC who previously received half-dose PDT and found that as many as 32 patients had MNV visible on OCT-A with a mean interval of 40 months between half-dose PDT and follow-up OCT-A imaging. The authors also found that the patients who developed MNV were generally older, received PDT with a larger spot size, and had thinner SFCT at baseline compared to the patients who did not develop MNV.
Whether patients with CSC who receive multiple PDT treatments have a higher risk of adverse effects is currently unknown. However, a recent retrospective study by Pauleikhoff and colleagues involving 55 patients with cCSC who underwent a bilateral half-dose PDT found that 73 of the 110 eyes (66 %) had complete SRF remission 5 months after treatment, with no adverse events reported.
Taken together, these studies provide extensive evidence suggesting that PDT is a safe and effective treatment option for CSC.
Conventional laser photocoagulation
Focal continuous-wave thermal laser photocoagulation (also known as continuous wave laser, focal laser, and conventional laser) was traditionally used to treat extrafoveal leakage in CSC; this treatment was typically performed using a diode laser or argon laser, but has also been performed using a krypton laser or xenon laser. With conventional laser photocoagulation, the focal leakage points on FA are targeted. Importantly, conventional laser photocoagulation is suitable only for treating extrafoveal leakage points, as adverse events such as scotoma, vision loss, reduced contrast sensitivity, and/or MNV can occur at the treated area due to damage to the neuroretina-RPE-Bruch’s membrane at the treatment site.
Although conventional laser photocoagulation can reduce the duration of SRF, studies found no significant difference in BCVA between treated patients and untreated patients with unspecified CSC. In another study from the pre-OCT era, Burumcek et al. found that the time to reach complete SRF resolution was shorter in eyes with persistent CSC that were treated with conventional laser photocoagulation on the focal leakage point compared to untreated eyes. Moreover, the prevalence of SRF recurrence after a mean follow-up period of 4.8 years was significantly lower in the conventional laser photocoagulation‒treated group, (0 out of 29 eyes) compared to 7 out of 16 eyes in the untreated group. A RCT conducted by Verma and colleagues found that using a diode laser yielded a superior outcome compared to using an argon laser in terms of BCVA improvement measured in 30 patients with unspecified CSC.
Navigated conventional laser photocoagulation has been suggested to provide a safe and effective continuous-wave laser modality for treating CSC. Using navigated conventional laser photocoagulation, the information obtained from fundus photography and FA imaging is integrated in order to identify the area to be treated. Using this integrated information, a computer then performs automated photocoagulation using a 532-nm laser. Several studies applied navigated conventional laser photocoagulation to the focal leakage point on FA and yield complete SRF resolution rates of 75–100 % among patients with CSC, although BCVA outcome varied.
A recent retrospective chart review of 62 patients with CSC who were treated with conventional laser photocoagulation and 29 patients who were treated with full-dose PDT found that the patients treated with conventional laser photocoagulation took longer to reach SRF resolution compared to the patients treated with full-dose PDT (1.8 vs. 1.2 months, respectively, p = 0.005); however, at their 3-year follow-up they found no difference in BCVA between the 2 treatment groups. In addition, the recurrence rate in the PDT-treated group was only 10 %, compared to 30 % in the conventional laser photocoagulation‒treated group. In a recent retrospective study, Yamada-Okahara and found a significantly higher rate of complete SRF resolution 3 months after treatment in 42 patients who received half-fluence PDT compared to 7 patients who received conventional laser photocoagulation (81 % vs. 29 %, respectively). A long-term prospective RCT that compared conventional laser photocoagulation to no treatment found no difference in recurrence rate or BCVA in 69 patients with undefined CSC measured 6–12 years after treatment.
Zhou and colleagues randomized 110 patients with aCSC to received treatment with either 577-nm HSML or conventional laser photocoagulation. Three months after treatment, 73 % of the patients in the HSML group had complete SRF resolution, compared to 89 % of the patients treated with a conventional laser photocoagulation (p = 0.029); at 6 months, the complete SRF rate was similar between the 2 (86 % vs. 93 %, respectively, p = 0.221). Moreover, 6 months after treatment, the authors found no significant difference in BCVA. Another RCT compared HSML to conventional laser photocoagulation in 88 patients with unspecified CSC and found that complete SRF resolution rates of 64 % and 82 %, respectively, 12 weeks after treatment; however, this difference was not significant (p = 0.056). In addition, at 12 weeks the gain in BCVA was similar between the HSML and conventional laser photocoagulation groups, with average gains of 6 and 7 ETDRS letters, respectively (the p-value for non-inferiority was 0.0026). In contrast, Piasecka et al. found a lower rate of complete SRF resolution rate at 12 months in patients treated with HSML compared to patients treated with conventional laser photocoagulation (74 % and 88 %, respectively); however, the increase in BCVA was larger in the HSML group compared to the conventional laser photocoagulation group. Lastly, Maruko et al. found that in contrast to PDT treatment, treating CSC with conventional laser photocoagulation did not change SFCT. This finding may be explained by the underlying choroidal abnormalities in CSC, which may not be treated as effectively using conventional laser photocoagulation.
In conclusion, when PDT—the preferred treatment option due to its favorable outcome—is not available or not indicated, conventional laser photocoagulation can be considered for treating extramacular focal leakage points.
Subthreshold micropulse laser
With subthreshold micropulse laser treatment, the aim is to selectively target the RPE without causing visible tissue damage. Micropulse laser treatment was first used as a treatment for macular edema in patients with diabetic retinopathy or retinal vein occlusion. This treatment was later proposed for CSC. Although micropulse laser treatment has been used for over 2 decades, its mechanism of action remains poorly understood. During treatment, photons are delivered to the retina in a train of brief (100–500 μs duration) laser pulses, thus allowing heat to dissipate between pulses. Using this approach, the temperature of the tissue stays below the threshold at which cellular proteins start to denature, and laser-induced burns are avoided. Chromophores present in the RPE (primarily melanin) absorb the photons’ energy, which is dissipated as heat. When applied at sublethal levels, this treatment is believed to increase the expression of heat shock proteins; because this increase in expression is believed to restore cellular function in the RPE, it can be particularly relevant for treating chorioretinal diseases such as CSC.
With high-threshold subthreshold micropulse laser (HSML), the diffusion of heat to surrounding tissues is minimized, thereby preventing tissue coagulation and scarring. To treat CSC using HSML, the laser spots are typically targeted to the hyperfluorescent abnormalities seen on ICGA (although some groups target the focal leakage points visible on FA). The laser spots are packed closely together in a dense pattern, with adjacent, non-overlapping spots focused on the designated treatment area.
A wide combination of micropulse laser strategies and laser types have been studied and recommended in interventional studies in CSC, which complicates comparisons between studies and makes reproducing the putative benefits difficult. Laser settings that can be adjusted include the wavelength, duty cycle (the percentage of time that the laser is actively emitting laser light), power (i.e., laser intensity), treatment spot size, and pulse duration (defined as the interval between each pulse cycle). To date, 810-nm, 577-nm, 532-nm, and 527-nm wavelengths have been studied. With respect to duty cycle, studies have used values ranging from 5 % to 15 %. Power levels ranging from 90 mW to 1800 mW have been used, with spot size ranging from 100 μm to 200 μm. Lastly, pulse duration ranged from 100 ms to 300 ms.
HSML in acute CSC. Several studies have investigated the use of HSML for the treatment of aCSC. In a prospective study, Inagaki et al. compared HSML with a 5% duty cycle to conventional laser photocoagulation in 49 patients with aCSC and found that 89% and 91% of patients in each group, respectively, achieved complete SRF resolution after a mean follow-up of 8 months. Similarly, Scholz and colleagues reported a complete SRF resolution rate of 82% at 12 weeks and 95% at 6 months after HSML treatment in 60 patients with aCSC. In a retrospective study, Abd Elhamid found a higher rate of complete SRF resolution in patients with aCSC who were treated with 577-nm HSML at a lower power setting (90 mW) compared to patients treated at a higher power setting (120 mW) (91% versus 81%, respectively), although this difference was not significant.
HSML in chronic CSC. The results of HSML treatment for cCSC are less favorable than for aCSC. As mentioned above, the PLACE trial showed that half-dose PDT was superior to HSML in terms of complete SRF resolution, with 67% and 29% of patients, respectively, achieving SRF resolution after a mean follow-up of 7–8 months. In addition, the long-term follow-up study of the PLACE trial found that only 53% of the patients who achieved complete SRF resolution after HSML still had a resolved SRF 1 year later, compared to 93% of patients treated with half-dose PDT. In addition, a retrospective study by Trinh et al. that included 38 eyes with cCSC found a complete SRF resolution rate of only 24% after a mean follow-up of 8 months. Similarly, in a case series of 24 eyes with cCSC, Venkatesh et al. reported a complete SRF resolution rate of 42% after 6 months.
Other studies have found more favorable results. For example, a retrospective study of 23 patients with cCSC found a complete SRF resolution rate of 83% after 12 months, and another retrospective study found a complete SRF resolution rate of 73% in 30 patients with cCSC. A prospective study involving 28 patients with cCSC treated with HSML found a complete SRF resolution rate of 71% after 12 months.
Several studies have compared HSML to half-dose PDT. A retrospective study by Chew et al. involving 68 patients with cCSC found that the patients treated with HSML had a higher rate of complete SRF resolution compared to patients treated with half-dose PDT (84% versus 76%, respectively) after a mean follow-up of 8 months, although this difference was not significant. In another retrospective study of 52 patients with cCSC, Breukink et al. found that after 1 year, the complete SRF resolution rate was higher in the half-dose PDT group (83%) compared to the HSML group (57%).
In conclusion, although some studies have reported favorable results for HSML in the treatment of cCSC, the results of the PLACE trial and its follow-up studies suggest that half-dose PDT is a superior treatment option.
Safety of subthreshold micropulse laser. HSML is generally considered a safe treatment, with few reported adverse events. The most common adverse event is a transient increase in SRF, which has been reported in up to 15% of cases. Other rare adverse events include a transient scotoma, a transient increase in metamorphopsia, and the development of MNV.
Treatment with oral medication
A number of oral medications have been investigated for the treatment of CSC, including mineralocorticoid receptor antagonists, rifampicin, methotrexate, finasteride, and aspirin.
Mineralocorticoid receptor antagonists. As discussed above, the mineralocorticoid receptor (MR) has been implicated in the pathophysiology of CSC. Two MR antagonists, spironolactone and eplerenone, have been studied for the treatment of CSC.
Spironolactone is a non-selective MR antagonist that also has anti-androgenic effects. In a prospective, randomized, placebo-controlled trial involving 38 patients with cCSC, Bousquet et al. found no significant difference in the rate of complete SRF resolution between patients treated with spironolactone (25 mg/day) and patients treated with placebo (25% versus 21%, respectively) after 3 months. In contrast, a retrospective study by Ghadiali et al. involving 60 patients with cCSC found a complete SRF resolution rate of 57% in patients treated with spironolactone (50 mg/day) after a mean follow-up of 6 months.
Eplerenone is a selective MR antagonist with fewer anti-androgenic effects than spironolactone. As mentioned above, the VICI trial, a large, multicenter, randomized, placebo-controlled trial involving 114 patients with cCSC, found no significant difference in the rate of complete SRF resolution between patients treated with eplerenone (25 mg/day for 1 week, then 50 mg/day) and patients treated with placebo (11% versus 19%, respectively) after 12 months. Similarly, the SPECTRA trial found that half-dose PDT was superior to eplerenone for the treatment of cCSC.
In conclusion, the available evidence does not support the use of mineralocorticoid receptor antagonists for the treatment of CSC.
Rifampicin. Rifampicin is an antibiotic that also has anti-inflammatory and anti-angiogenic properties. A prospective, randomized, placebo-controlled trial involving 34 patients with cCSC found no significant difference in the rate of complete SRF resolution between patients treated with rifampicin (300 mg/day) and patients treated with placebo (29% versus 24%, respectively) after 3 months.
Methotrexate. Methotrexate is an immunosuppressive drug that has been used to treat a variety of inflammatory and autoimmune diseases. A retrospective study of 12 patients with cCSC treated with low-dose methotrexate (7.5–15 mg/week) found a complete SRF resolution rate of 58% after a mean follow-up of 6 months.
Finasteride. Finasteride is a 5-alpha-reductase inhibitor that is used to treat benign prostatic hyperplasia and male pattern baldness. A small case series of 3 patients with cCSC who were treated with finasteride (5 mg/day) reported complete SRF resolution in all 3 patients after 3 months.
Aspirin. Aspirin has anti-platelet and anti-inflammatory properties. A retrospective study of 25 patients with cCSC who were treated with low-dose aspirin (100 mg/day) found a complete SRF resolution rate of 64% after a mean follow-up of 6 months.
In conclusion, there is insufficient evidence to support the use of any of these oral medications for the treatment of CSC.
Treatment for bullous CSC
Bullous CSC is a rare and severe form of CSC that is characterized by a large, bullous neurosensory detachment. Treatment is often challenging, and the visual prognosis is generally poor. PDT has been used to treat bullous CSC, with some success. In a case series of 5 patients with bullous CSC, 4 patients had complete SRF resolution after treatment with full-dose PDT. In another case series of 3 patients with bullous CSC, all 3 patients had complete SRF resolution after treatment with half-dose PDT.
Treatment of CSC in pregnancy
CSC can occur during pregnancy, and is thought to be related to hormonal changes. In most cases, the SRF resolves spontaneously after delivery, and the visual prognosis is generally good. Treatment is usually not necessary. However, if the vision is severely affected, treatment with half-dose PDT may be considered.
Treatment of CSC complicated by macular neovascularization
MNV is a rare complication of CSC, occurring in approximately 1–2% of cases. Treatment is aimed at closing the neovascular complex and resolving the associated SRF. Intravitreal anti-VEGF therapy is the first-line treatment for MNV in CSC. In a retrospective study of 12 patients with CSC and MNV, 10 patients (83%) had complete SRF resolution after a mean of 3 intravitreal injections of bevacizumab. In another retrospective study of 10 patients with CSC and MNV, all 10 patients had complete SRF resolution after a mean of 2 intravitreal injections of ranibizumab.
If anti-VEGF therapy is not effective, PDT may be considered. In a case series of 5 patients with CSC and MNV who were treated with half-dose PDT, 4 patients (80%) had complete SRF resolution.
Conclusion
CSC is a complex chorioretinal disease with a wide spectrum of clinical presentations. Although aCSC often resolves spontaneously, cCSC can lead to permanent vision loss. The pathophysiology of CSC is not fully understood, but choroidal dysfunction appears to play a central role. Multimodal imaging is essential for diagnosis and for guiding treatment.
Half-dose PDT is the most effective treatment for cCSC, and is superior to both HSML and oral eplerenone. Half-dose PDT is also a safe and effective treatment for aCSC, although observation is a reasonable option in many cases. Conventional laser photocoagulation can be considered for extrafoveal leakage in cases where PDT is not available. There is insufficient evidence to support the use of any oral medications for the treatment of CSC.
For bullous CSC, PDT is a viable treatment option. For CSC in pregnancy, observation is the preferred approach, with PDT reserved for severe cases. For CSC complicated by MNV, intravitreal anti-VEGF therapy is the first-line treatment, with PDT as a second-line option.
Further research is needed to better understand the pathophysiology of CSC and to develop new and more effective treatments. A universally accepted classification system for CSC is also needed to facilitate research and to guide clinical practice.
- Feenstra, H.M.A., van Dijk, E.H.C., Cheung, C.M.G., Ohno-Matsui, K., Lai, T.Y.Y., Koizumi, H., … Boon, C.J.F. (2024). Central serous chorioretinopathy: An evidence-based treatment guideline. Progress in Retinal and Eye Research, 101, 101236. https://doi.org/10.1016/j.preteyeres.2023.101236