Laser Fundamentals
- Definition: Laser = Light Amplification by Stimulated Emission of Radiation.
- Components:
- Optical Resonator: Comprises mirrors forming a cavity where light circulates.
- Gain Medium: Amplifies light (e.g., laser crystal, gas, or semiconductor).
- Pumping Mechanism: Supplies energy to the gain medium (optical or electrical pumping).
- Stimulated Emission:
- A photon stimulates an excited atom to emit another photon with identical phase, direction, and wavelength.
- Requires population inversion (more atoms in excited state than lower state) achieved via excitation sources (e.g., lamps, electric discharges, or other lasers).
- Laser Beam Characteristics:
- Monochromatic: Single wavelength, preventing chromatic aberration.
- Coherent: Photons in phase, allowing precise focusing in space and time.
- Pulsing Methods: Electronic shutters (ms), pulsed flash lamps (µs), Q-switching (ns), or mode locking (fs).
Laser-Tissue Interactions
- Dependence: Interactions vary based on:
- Tissue Properties: Spectral absorption, scattering, and conductivity.
- Laser Parameters: Wavelength, spot size, pulse energy, intensity, and duration.
- Three Main Interaction Types:
- Photochemical:
- Low-energy, wavelength-specific reactions produce free radicals, causing cellular damage.
- Applications:
- Photodynamic Therapy (PDT): Uses verteporfin to target choroidal neovascularization (e.g., in AMD). Light-activated chromophore induces chemical reactions at low irradiance to avoid thermal damage.
- Corneal Collagen Cross-Linking (CXL): Riboflavin (photosensitizer) with UV-A (370 nm) increases corneal rigidity for keratoconus or ectasia via reactive oxygen species and collagen bond formation.
- Excimer Lasers: Photoablation (UV light, ns pulses) breaks corneal collagen bonds for precise incisions (e.g., LASIK, phototherapeutic keratectomy) with minimal collateral damage.
- Photothermal:
- Laser energy increases molecular vibration, raising tissue temperature.
- Effects depend on temperature and exposure:
- ~60°C: Protein denaturation and coagulation.
- ~300°C: Tissue vaporization.
- Applications:
- Retinal Photocoagulation: Uses green Nd:YAG (532 nm) or yellow semiconductor (577 nm) lasers to coagulate RPE, choroid, and blood vessels (melanin and hemoglobin as chromophores). Treats retinovascular diseases (e.g., diabetic retinopathy).
- Subthreshold Micropulse Laser: Low-energy millisecond pulses selectively target RPE, sparing neurosensory retina, minimizing scarring. Used for diabetic macular edema and other retinovascular conditions.
- Photovaporization: High-energy lasers (e.g., CO2 laser, far infrared) vaporize tissue and coagulate vessels, creating a bloodless field (e.g., for vascular pathologies).
- Photomechanical/Ionizing:
- High-irradiance, short-pulse (ns/ps) Nd:YAG lasers (1064 nm) create plasma, leading to shock/acoustic waves that disrupt tissue.
- Applications:
- Photodisruption: Used for posterior capsular opacification (post-cataract surgery), vitreous membrane disruption, and peripheral iridotomy (for angle-closure glaucoma). No pigmentation required, only precise focusing.
- Photochemical:
Ophthalmic Suitability
- Eye Anatomy: Optimized for light transmission, making lasers ideal for precise targeting.
- Wavelength Specificity: Matches tissue chromophores (e.g., melanin in RPE, hemoglobin in vessels) for effective therapy.
- Pulse Duration: Short pulses (ns–fs) enable high-precision ablation with minimal thermal spread.
Clinical Applications
- Anterior Segment:
- Excimer laser: LASIK, PRK, phototherapeutic keratectomy.
- CXL: Keratoconus, corneal ectasia.
- Nd:YAG: Peripheral iridotomy, capsulotomy.
- Posterior Segment:
- PDT: Choroidal neovascularization (e.g., AMD).
- Retinal photocoagulation: Diabetic retinopathy, retinal vein occlusion.
- Subthreshold micropulse: Diabetic macular edema, central serous chorioretinopathy.
- Challenges:
- Micropulse Titration: No visible treatment effect increases risk of undertreatment; guidelines exist to optimize outcomes.
- Thermal Damage: Careful parameter selection (pulse duration, spot size) minimizes collateral damage.
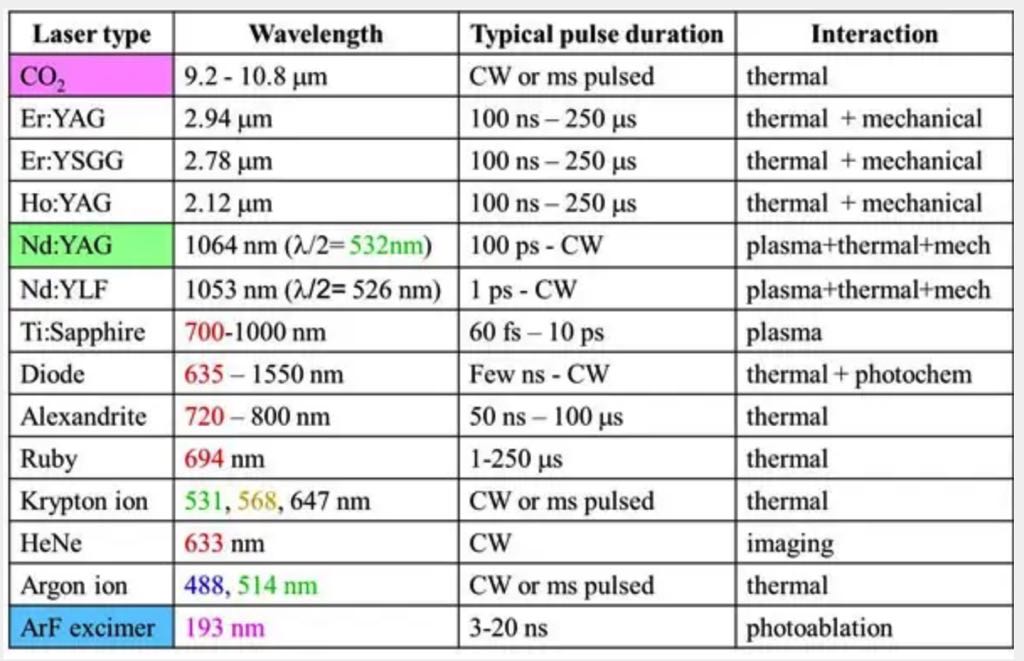
Key Historical and Modern Lasers
- Historical: Ruby (694 nm), argon (488/514 nm), krypton (647 nm).
- Modern: Green Nd:YAG (532 nm), yellow semiconductor (577 nm), Nd:YAG (1064 nm), excimer (UV), CO2 (far infrared).
Citation
Elsayed MEA, Kozak I. Basics of Laser Use in Ophthalmology. In: Grzybowski A, et al., editors. Retina Lasers in Ophthalmology. Springer Nature Switzerland AG; 2023. doi:10.1007/978-3-031-25779-7_3