- Definition and Classification of Type 3 MNV:
- Type 3 macular neovascularization (MNV) is a distinct form of neovascular age-related macular degeneration (AMD) originating from the retinal vasculature, specifically the deep capillary plexus (DCP).
- Accounts for 10-30% of neovascular AMD cases in White populations and 5-10% in Asian populations.
- Characterized by intraretinal neovascularization, differing from type 1 (sub-RPE) and type 2 (subretinal) MNV.
- Epidemiology and Risk Factors:
- Typically affects individuals older than 75 years.
- Twice as common in women compared to men.
- Bilateral involvement is common, with a high risk of progression to macular atrophy.
- Genetic risk alleles are associated with type 3 MNV.
- Pathogenesis:
- Hypoxia is a key driver, resulting from retinal pigment epithelium (RPE) disruption, photoreceptor loss, and choriocapillaris degeneration.
- Neovascularization arises from the DCP, accompanied by activated Müller glia infiltrating sub-RPE basal laminar deposits (BLamD).
- Dysregulation of angiogenic (e.g., VEGF) and angiostatic factors plays a critical role.
- Basal linear deposits (BLinD) and BLamD create barriers to retinal oxygenation, exacerbating hypoxia.
- The “oil spill” hypothesis highlights aging Bruch’s membrane (BrM) changes as a contributor to AMD pathogenesis.
- Clinical Features and Prognosis:
- High risk of bilateral involvement and progression to macular atrophy, a critical prognostic factor.
- Often presents with intraretinal hemorrhage and fluid (IRHF), detectable on multimodal imaging.
- Type 3 MNV is a bilateral condition with a worse visual prognosis compared to other MNV types due to atrophy.
- Imaging and Diagnosis:
- Multimodal imaging (e.g., OCT, OCTA) is essential for diagnosis, showing intraretinal neovascularization and exudation.
- OCTA reveals pronounced signal attenuation in the choriocapillaris and reduced choroidal thickness in type 3 MNV.
- Differentiate type 3 MNV from deep retinal age-related microvascular anomalies (DRAMA), which mimic precursor lesions but have low neovascular potential and may not require anti-angiogenic treatment.
- Differential Diagnosis:
- DRAMA presents with similar imaging features (exudative retinal microvascular anomalies in the DCP with adjacent IRHF) but does not typically progress to MNV.
- Accurate differentiation is critical, as DRAMA may not require the same aggressive treatment as type 3 MNV.
- Precursor lesions of type 3 MNV may be confused with DRAMA, necessitating careful longitudinal monitoring.
- Management Implications:
- Recognition of type 3 MNV is critical for tailoring treatment, as it differs from type 1 and type 2 MNV in response to anti-VEGF therapy.
- The “pre-proliferative” stage (non-neovascular intraretinal exudation) may require monitoring rather than immediate intervention.
- Anti-VEGF therapy is the mainstay for active type 3 MNV, but treatment protocols may vary based on disease stage and progression.
- Nomenclature and Taxonomy:
- Historically polyonymous due to debates over its retinal vs. choroidal origin; now confirmed as retinal in origin.
- The term “type 3 disease” or “type 3 vasculopathy” encompasses a spectrum, including a pre-proliferative stage with non-neovascular exudation.
- High-Yield Exam Points:
- Type 3 MNV originates from the retinal deep capillary plexus (DCP), not the choroid, unlike type 1 and type 2 MNV.
- Bilateral involvement and progression to macular atrophy are key prognostic features.
- Hypoxia and VEGF dysregulation are central to pathogenesis.
- Differentiate type 3 MNV from DRAMA using multimodal imaging, as management differs significantly.
- Women over 75 are at higher risk, and genetic factors contribute to susceptibility.
Citation
Faes, L., Bijon, J., Bacci, T., & Freund, K. B. (2025). Review of type 3 macular neovascularization in age-related macular degeneration: no DRAMA (Deep Retinal Age-related Microvascular Anomalies). Eye, 39, 870–882. https://doi.org/10.1038/s41433-024-03343-3
DRAMA refers to a specific type of retinal change that manifests as microvascular anomalies within the deep capillary plexus of the retina. This condition often occurs in the context of non-neovascular AMD and can present in two primary forms:
-
Round-shaped capillary dilations, which exhibit varying reflectivity and are localized in the inner nuclear layer.
-
Downward outpouchings, typically multiple, that extend into the Henle fiber layer and demonstrate reflectivity similar to normal retinal capillaries
Clinical Significance
The identification of DRAMA is crucial as it can sometimes masquerade as type 3 macular neovascularization (MNV), complicating diagnosis and treatment strategies. Although DRAMA lesions are non-neovascular, they can still lead to intraretinal exudation, which may vary over time without progressing to MNV.
This characteristic poses a challenge for treatment, as traditional therapies for exudative conditions like anti-VEGF injections may not always be effective for DRAMA lesions.
Diagnostic Techniques
Recent advancements in optical coherence tomography (OCT) and OCT angiography (OCTA) have significantly enhanced the ability to visualize and characterize DRAMA. These imaging techniques help differentiate DRAMA from other retinal conditions, particularly MNV, by providing detailed insights into the vascular architecture and abnormalities present in the deep retinal layers
Research has established protocols using volume rendering of OCT data to assess capillary features, allowing for more accurate diagnosis and understanding of disease progression.
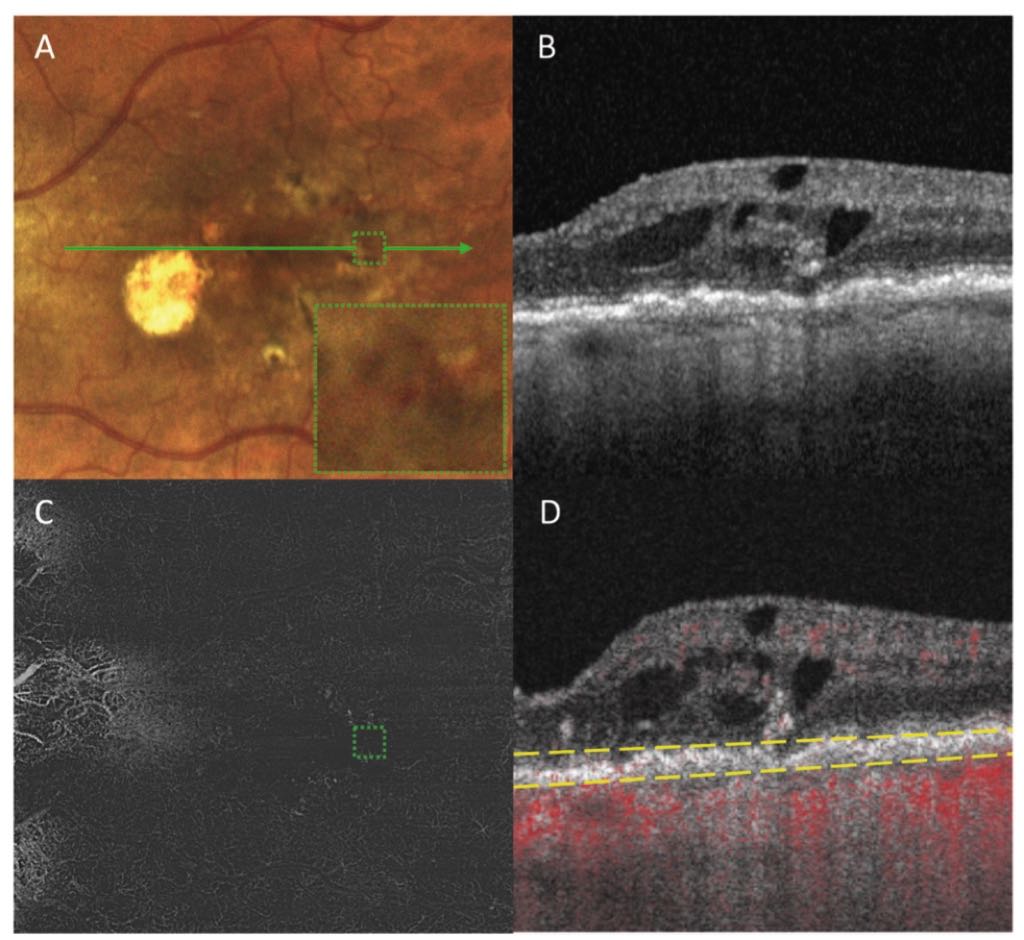
Multimodal imaging of the left eye of a 98-year-old male with a deep retinal age-related microvascular anomaly (DRAMA) and geographic atrophy.
Conclusion
DRAMA represents an important aspect of retinal pathology in the aging population, particularly among patients dealing with AMD. Ongoing research is necessary to further elucidate the clinical implications of DRAMA, improve classification, and optimize treatment approaches for affected patients. As our imaging capabilities continue to advance, precise identification and differentiation from other similar retinal disorders will likely become more reliable.