Risk of Progression of Non-Proliferative to Proliferative Diabetic Retinopathy Following Cataract Surgery
– Study Overview:
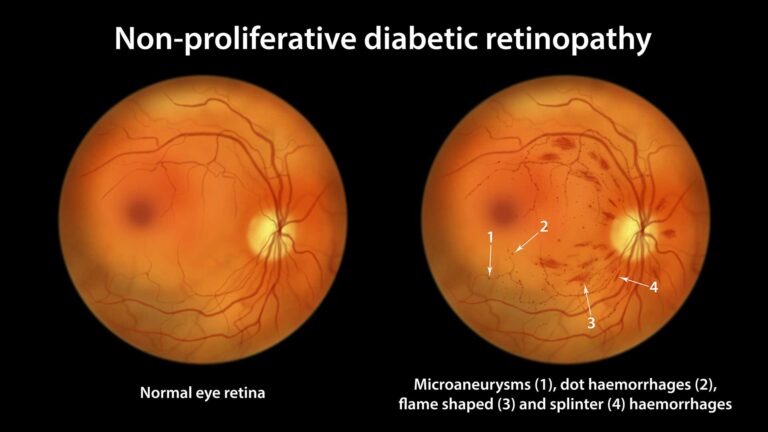
– Retrospective analysis using the TriNetX US Collaborative research network (2004–2024), focusing on modern phacoemulsification cataract surgery in patients with type 2 diabetes (T2D) and non-proliferative diabetic retinopathy (NPDR).
– Purpose: To assess progression from NPDR to proliferative diabetic retinopathy (PDR) within 1 year post-cataract surgery, addressing conflicting literature on modern surgical techniques.
– Study Design and Population:
– Included patients ≥18 years with T2D and NPDR (with or without diabetic macular edema [DME]) identified via ICD-10 codes.
– Exclusion criteria: Type 1 diabetes, sickle cell retinopathy, prior PDR, vitreous hemorrhage (VH), panretinal photocoagulation (PRP), secondary glaucoma, vitrectomy, complex cataract surgery (CPT 66982), or intraoperative/postoperative complications (e.g., pseudophakic bullous keratopathy).
– Study cohort: Patients undergoing routine cataract surgery (CPT 66984) for age-related cataracts in the right or left eye.
– Control cohort: NPDR patients receiving ophthalmology services but no cataract surgery.
– Propensity score matching (PSM) balanced for age, gender, ethnicity, race, HbA1c, NPDR stage, comorbidities (e.g., diabetic nephropathy, hypertension), and prior intravitreal injections (e.g., anti-VEGF).
– Main Outcome Measures:
– 1-year risk of:
– PDR without complications (ICD-10: E11.3511, E11.3593, etc.).
– Vitreous hemorrhage (VH) (H43.11, H43.13).
– Tractional retinal detachment (TRD) or combined tractional and rhegmatogenous retinal detachment (CTRD) (E11.3521, E11.3543, etc.).
– Composite outcome (any of the above).
– Key Findings:
– Right Eye Analysis (n=3589 per cohort post-PSM):
– Increased 1-year risk of PDR without complications (HR 1.45; 95% CI 1.09–1.92), VH (HR 1.92; 95% CI 1.13–3.25), and composite outcome (HR 1.49; 95% CI 1.13–1.96) in operated eyes.
– No significant difference in TRD/CTRD risk (HR 0.76; 95% CI 0.17–3.39, P>0.05).
– Left Eye Analysis (n=3616 per cohort post-PSM):
– Increased 1-year risk of PDR without complications (HR 1.58; 95% CI 1.17–2.13), VH (HR 2.12; 95% CI 1.23–3.66), and composite outcome (HR 1.60; 95% CI 1.21–2.13) in operated eyes.
– No significant difference in TRD/CTRD risk (HR 5.09; 95% CI 0.59–43.55, P>0.05).
– Sensitivity Analysis (T2D ≥5 years, n=2488 per cohort):
– Confirmed increased 1-year risk of PDR without complications (HR 1.52; 95% CI 1.06–2.19), VH (HR 2.50; 95% CI 1.20–5.20), and composite outcome (HR 1.75; 95% CI 1.22–2.51).
– No significant difference in TRD/CTRD risk (HR 1.50; 95% CI 0.25–8.99, P>0.05).
– No increased risk for TRD/CTRD across all analyses, consistent with TRD being a late PDR complication unlikely to occur within 1 year of initial PDR progression.
– Pathophysiology:
– Cataract surgery disrupts the blood-aqueous barrier (BAB), causing a pro-inflammatory state more pronounced in diabetic eyes (evidenced by greater aqueous flare).
– Angiogenic imbalance: Post-surgery, diabetic eyes show increased VEGF and hepatocyte growth factor (HGF) and decreased pigment epithelial-derived growth factor (PEDF), potentially driving PDR progression.
– Phacoemulsification causes less BAB disruption and inflammation than older techniques (ICCE, ECCE), yet still associated with PDR risk.
– Clinical Implications:
– Modern cataract surgery increases 1-year risk of NPDR to PDR progression, necessitating close postoperative follow-up with dilated fundus exams (DFE), especially in T2D patients with NPDR.
– No standard DFE protocol post-cataract surgery, but 83% of ophthalmologists perform DFE within 4 months; stronger advocacy for DFE in diabetic patients.
– Findings inform shared decision-making, highlighting need for preoperative counseling on PDR risk.
– Comparison to Prior Literature:
– Older techniques (ICCE, ECCE) consistently linked to DR progression due to greater inflammation.
– Conflicting data on phacoemulsification: Some studies (Mittra, Krepler, Squirrell, Romero-Aroca) found no increased risk, while others (Hong, Jeng) reported elevated DR risk, often in DR-naïve or mixed cohorts.
– This study’s large sample size (n=7178 right eye, n=7232 left eye post-PSM) and focused NPDR cohort provide robust evidence compared to smaller, heterogeneous prior studies.
– Lee et al. meta-analysis (2024) supports increased DR risk post-phacoemulsification but notes limitations in prior study designs.
– Strengths:
– Large, multicenter cohort with comprehensive PSM for demographic, systemic (e.g., HbA1c, nephropathy), and ocular factors (e.g., NPDR stage, anti-VEGF use).
– Sensitivity analysis for T2D duration (≥5 years) strengthens findings.
– Excluded complex cases to reduce confounding from surgical complications.
– Limitations:
– Database limitations: No visual acuity data, surgeon experience, or surgery duration; reliant on ICD/CPT coding, risking miscoding.
– Separate eye analyses (right/left) due to TriNetX platform limitations, preventing inter-eye correlation assessment.
– Unable to account for timing of anti-VEGF therapy relative to surgery.
– Small differences in matched variables (SMD <0.1) may still introduce bias.
These points emphasize increased PDR risk post-cataract surgery, pathophysiology (BAB disruption, VEGF), need for DFE follow-up, and study strengths/limitations.