Clinical Description
- Definition: Acquired retinal arterial macroaneurysms are fusiform or round dilations of retinal arterioles, typically in the posterior fundus within the first three orders of arteriolar bifurcation.
- Common Location: Often at arteriolar bifurcations or arteriovenous crossings, with the supratemporal artery most frequently involved due to visual impairment risk.
- Demographics: Predominantly affects women, usually unilateral (10% bilateral), most common in the sixth and seventh decades of life.
- Prevalence: Estimated at 1 in 9000 (Beijing Eye Study).
- Associations: Strongly linked to hypertension, arteriosclerotic cardiovascular disease, and serum lipid/lipoprotein abnormalities. Systemic evaluation for these conditions is critical.
- Symptoms: Asymptomatic if the macula is spared; otherwise, decreased central visual acuity due to retinal edema, exudation, or hemorrhage.
- Hemorrhage Types: Can occur in subretinal space, intraretinal, beneath the internal limiting membrane, or into the vitreous.
- Hourglass hemorrhages are characteristic.
- Complications: Vitreous hemorrhage may lead to angle-closure glaucoma; subretinal hemorrhage may mimic malignant melanoma or age-related macular degeneration.
Diagnosis
- Fluorescein Angiography (FA):
- Hypofluorescence due to hemorrhage blocking fluorescence; hyperfluorescence of the macroaneurysm itself.
- May fail to detect macroaneurysm if obscured by dense hemorrhage.
- Indocyanine Green Angiography (ICGA):
- Useful for dense hemorrhages due to near-infrared penetration.
- Shows pulsatile lesions contiguous with the arterial wall, pathognomonic for macroaneurysms.
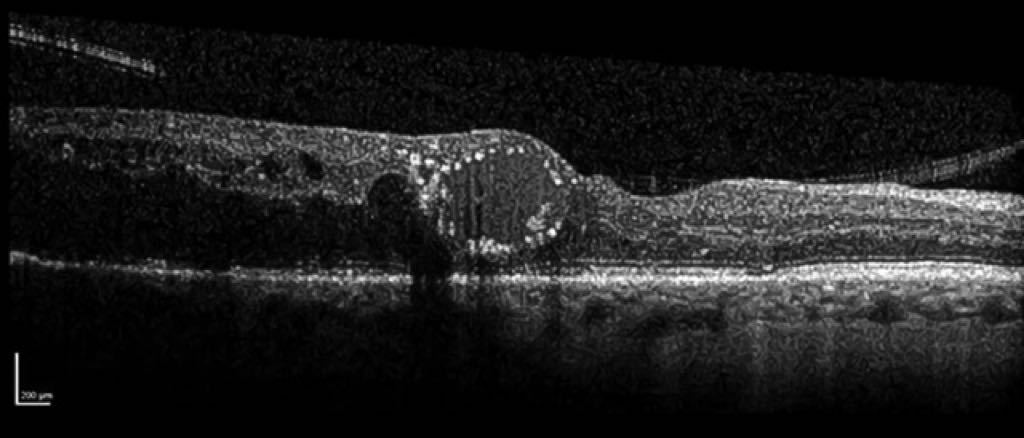
- Optical Coherence Tomography (OCT):
- Detects foveal edema, subretinal hemorrhage, and structural retinal changes.
- OCT angiography is noninvasive, effective for locating macroaneurysms, and an alternative to FA/ICGA.
- Histopathology: Shows arteriolar distension, fibroglial proliferation, dilated capillaries, extravasated blood, lipoidal exudates, and hemosiderin.
- Pearl Necklace Sign: Hyperreflective dots around cystoid spaces in the outer plexiform layer, seen in exudative macular diseases (not specific to macroaneurysms).
- Hyperreflective dots arranged as a contiguous ring along the inner wall of cystoid spaces on the macular OCT scan, termed as the pearl necklace sign.
Natural Course
- Spontaneous Resolution: Many macroaneurysms thrombose and involute spontaneously, with clearing of macular exudate and good visual prognosis.
- Poor Outcomes: Exudative progression or subretinal hemorrhage can damage the foveal photoreceptor layer, leading to vision loss.
- Complications: Macular holes or dense submacular hemorrhage are associated with poor visual outcomes.
Treatment
- Observation: Preferred for asymptomatic cases or those with spontaneous resolution, as long-term visual outcomes may be comparable to treated cases.
- Intravitreal Bevacizumab:
- Improves visual acuity and reduces central retinal thickness in symptomatic cases.
- Faster resolution of hemorrhage and edema compared to observation.
- Vitrectomy:
- Used for macular hemorrhage; outcomes vary by hemorrhage location.
- Poor prognosis with dense submacular or intraretinal hemorrhage.
- Pneumatic Displacement: With or without tissue plasminogen activator, used for submacular hemorrhage.
- Laser Photocoagulation:
- Considered if lipid exudate threatens the fovea, but no clear evidence of benefit.
- Risk of arteriolar occlusion, especially if the distal arteriole supplies the macula.
- YAG Laser: Used for premacular hemorrhage.
- Surgical Excision: Rare, involves excision of macroaneurysm and drainage of submacular hemorrhage; limited evidence.
- Long-Term Outcomes: Treated and untreated patients often have comparable visual acuity, except in cases with macular holes or severe hemorrhage.
Differential Diagnosis
- Key Conditions: Diabetic retinopathy, retinal telangiectasia, retinal capillary angioma, cavernous hemangioma, malignant melanoma, and hemorrhagic pigment epithelial detachment (age-related macular degeneration).
Treatment Approaches for Retinal Arterial Macroaneurysm (RAMA) from Another Study
- Observation:
- Indicated for RAMAs without macular involvement or threat to the macula.
- In the study, 16 patients were observed; visual acuity (VA) remained stable (initial 0.48 logMAR vs. final 0.35 logMAR, p=0.08).
- 88% had some hemorrhage, 31% ruptured, but none involved the fovea.
- Laser Photocoagulation:
- Used for exudative RAMAs to induce thrombosis and reabsorb exudates.
- Techniques: Direct (targeting RAMA) or indirect (perilesional) coagulation; often combined.
- Parameters: Indirect (100-200 µm, 100-200 ms, moderate burns); Direct (200-500 µm, 200-500 ms, soft burns).
- Study outcomes: 15 patients; VA stable (initial 0.55 logMAR vs. final 0.59 logMAR, p=0.76). 33% lost VA, often due to comorbidities (e.g., CRVO, atrophic creep).
- Alternative: Subthreshold micropulse laser showed significant VA improvement in some studies (0.8 to 0.36 logMAR over 12 months).
- Vitrectomy:
- Indicated for hemorrhagic RAMAs with submacular or premacular bleeding.
- Techniques: May include recombinant tissue plasminogen activator (rtPA) injection (intravitreal/subretinal), internal limiting membrane (ILM) peeling, pneumatic displacement, or endotamponade (94% in study).
- Study outcomes: 18 patients; significant VA improvement (initial 1.8 logMAR vs. final 0.77 logMAR, p<0.001). Poor outcomes with macular hole (MH) formation (6% incidence).
- Timing: Short latency to surgery (mean 3.1 days) associated with better outcomes.
- Anti-VEGF Therapy:
- Effective for exudative RAMAs; bevacizumab closed 36/38 RAMAs in one study, with faster visual recovery but no long-term VA advantage (10 months).
- Minimal destructive side effects, making it suitable for perifoveal RAMAs.
- Not ideal for subfoveal/subretinal hemorrhage due to need for rapid blood removal.
Complications and Prognosis
- Complications:
- Macular Hole (MH): 6% incidence post-RAMA rupture; poor visual prognosis (VA: counting fingers to 20/400). Often discovered during vitrectomy, may be secondary to hemorrhage or ILM peeling.
- Subretinal hemorrhage: Can lead to retinal degeneration within weeks if untreated, potentially forming disciform fibrotic scars.
- Retinal detachment: Occurred in 3/18 vitrectomy cases during follow-up.
- Rare: Massive bleeding post-rtPA (1 case in study).
- Prognosis:
- Overall good visual prognosis: Mean VA stable over 3 years with individualized treatment (final VA: 0.58 logMAR, 63% retained reading acuity).
- Observation and laser groups maintained stable VA; vitrectomy group improved significantly despite worse initial VA.
- Poor outcomes associated with MH or severe surgical complications.
Management Guidelines
- Observation: For RAMAs not affecting/threatening the macula, monitored with OCT.
- Active Treatment: Indicated for actual or impending macular complications.
- Exudative RAMAs: Laser (direct/indirect) or anti-VEGF.
- Hemorrhagic RAMAs: Vitrectomy with rtPA, ILM peeling, or tamponade.
- Cardiovascular Workup: Essential due to association with hypertension and vascular disease.
- Individualized approach critical due to variable presentation and lack of randomized trials.
Associations
- Retinal Vein Occlusion (RVO): 27% of photocoagulation group had RVO history (same or fellow eye), suggesting RAMA as a manifestation of generalized vascular susceptibility rather than direct RVO causation.
- Other: Diabetic retinopathy, radiation retinopathy, central retinal artery occlusion noted in observation group.
Study Specifics
- Retrospective, single-center study (Kiel University, Germany, 2003-2013) with 49 RAMA cases.
- Groups: Observation (16), photocoagulation (15), vitrectomy (18).
- Follow-up: Mean 34 ± 23 months.
- Limitations: Retrospective design, non-standardized therapy, but provides detailed photocoagulation parameters and large surgical case series.
Citation
Koinzer S, Heckmann J, Tode J, Roider J. Long-term, therapy-related visual outcome of 49 cases with retinal arterial macroaneurysm: a case series and literature review. Br J Ophthalmol. 2015;99(10):1345-1353. doi:10.1136/bjophthalmol-2014-305884.