Pre-Operative Glycemic Control and Acute Endophthalmitis after Cataract Surgery
– Study Overview:
– Retrospective case-control study evaluating whether pre-operative hemoglobin A1c (HbA1c) predicts acute post-operative endophthalmitis within 42 days after cataract surgery in US Veterans with diabetes mellitus (DM).
– Conducted using the VA Corporate Data Warehouse (CDW), analyzing surgeries from 2010–2022.
– Study Population:
– Included 190,393 diabetic patients with HbA1c recorded 0–6 months prior to cataract surgery (81% of 233,815 diabetic patients undergoing surgery).
– Excluded: Age >105 years, HbA1c <2.8% or >25%, non-VA surgeries.
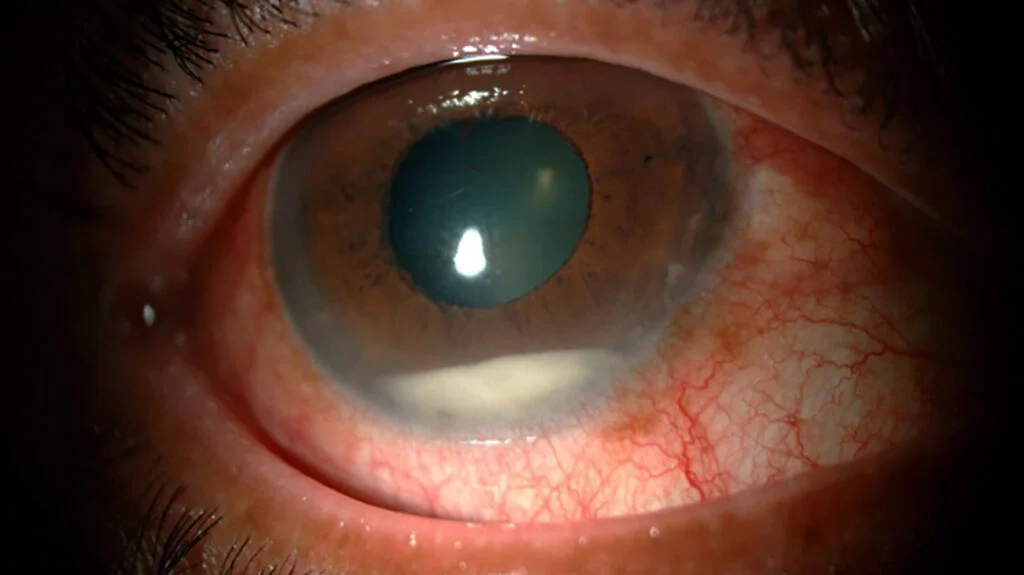
– Cases: 157 patients (0.08%) with confirmed acute endophthalmitis (verified by chart review).
– Controls: 190,173 patients without endophthalmitis.
– Subanalysis: Patients with HbA1c drawn 0–2 months prior (n=95,006 controls, n=78 cases).
– Methodology:
– Identified cataract surgeries via CPT codes (66982, 66983, 66984, etc.) and DM via ICD-9/10 codes (250.x, E10.x–E11.x).
– Endophthalmitis cases identified using CPT codes (e.g., intravitreal injection, vitrectomy) and ICD codes for panuveitis/endophthalmitis, confirmed by chart review to exclude false positives (e.g., uveitis, subsequent procedures).
– Statistical analysis:
– Univariable: T-tests for continuous variables (e.g., HbA1c), Chi-squared/Fisher’s exact for categorical variables.
– Multivariable: Logistic regression adjusting for age, sex, race, ethnicity, rural residence, resident surgeon involvement, diabetic retinopathy (DR) severity, same-day vitrectomy, DM duration, and HbA1c.
– Sensitivity analysis: Limited to routine extracapsular cataract extraction (CPT 66982, 66984).
– Key Findings:
– No association between pre-operative HbA1c and endophthalmitis:
– Mean HbA1c: 7.1 ± 1.4% (cases) vs. 7.3 ± 1.5% (controls) for 0–6 months (P=0.14).
– Subanalysis (0–2 months): 7.3 ± 1.2% (cases) vs. 7.4 ± 1.5% (controls) (P=0.31).
– Multivariable logistic regression: Adjusted OR 0.89 (95% CI 0.79–1.01, P=0.08) for 0–6 months; OR 0.90 (95% CI 0.74–1.06, P=0.22) for 0–2 months.
– Significant risk factors:
– Same-day vitrectomy: Associated with endophthalmitis (OR 4.68, 95% CI 1.66–10.28, P=0.007 for 0–6 months; less significant in 0–2 months subanalysis, P=0.08).
– Moderate/severe NPDR or PDR: Associated with endophthalmitis (OR 1.54, 95% CI 1.00–2.31, P=0.04 for 0–6 months; OR 2.15, 95% CI 1.19–3.74, P=0.009 for 0–2 months).
– No significant association with age, sex, race, ethnicity, rural residence, resident surgeon involvement, or DM duration.
– Sensitivity analysis (routine cataract surgeries) confirmed no HbA1c association.
– Clinical Implications:
– Pre-operative HbA1c not predictive of endophthalmitis risk, suggesting American Diabetes Association guideline (HbA1c <8% pre-surgery) may not apply to cataract surgery infection risk.
– Challenges routine HbA1c optimization before cataract surgery, supporting focus on other infection prevention strategies (e.g., sterile technique, perioperative antibiotics).
– Moderate/severe NPDR or PDR as a risk factor indicates DM severity (rather than short-term glycemic control) may influence endophthalmitis risk, aligning with studies using Diabetes Complications Severity Index (DCSI).
– Findings may reduce unnecessary pre-operative testing burdens, aligning with prior evidence that routine lab tests add little value for cataract surgery safety.
– Pathophysiology Context:
– DM increases infection risk via impaired innate immunity (e.g., reduced neutrophil chemotaxis, phagocytosis, cytokine dysfunction), corneal epithelial fragility, and impaired wound healing due to altered epidermal growth factor receptor signaling.
– HbA1c reflects 2–3-month glycemic control, unlike DCSI, which captures broader DM complications, potentially explaining why DM severity (e.g., DR) but not HbA1c predicts endophthalmitis.
– Comparison to Prior Literature:
– Supporting DM as risk factor: Studies (e.g., Hou et al., Kim et al.) found DM increases endophthalmitis risk, with DCSI >10 correlating with higher risk, focusing on long-term DM complications rather than HbA1c.
– Conflicting findings: Some studies (e.g., Montan et al., Javitt et al.) found no significant DM-endophthalmitis link, consistent with this study’s HbA1c findings.
– Unique contribution: This is the first study to directly assess pre-operative HbA1c as a predictor, distinguishing short-term glycemic control from overall DM severity.
– Strengths:
– Large national cohort (n=190,393) with chart review to confirm endophthalmitis cases, reducing coding errors.
– Recent data (2010–2022), covering modern cataract surgery practices pre- and post-COVID.
– Multivariable adjustment for confounders (e.g., DR severity, vitrectomy).
– Sensitivity and subanalyses (0–2 months, routine procedures) enhance robustness.
– Limitations:
– VA population: Predominantly male (97%), limiting generalizability to diverse populations.
– HbA1c timeframe: 0–6 months may not capture peri-operative glycemic status (e.g., ADA’s 4-hour pre-surgery guideline).
– Retrospective design: Reliant on coding accuracy, though mitigated by chart review.
– Rarity of endophthalmitis (0.08%) limits statistical power for some variables.
– Did not assess post-operative outcomes or other complications tied to HbA1c.
These points emphasize no HbA1c-endophthalmitis association, DM severity (NPDR/PDR) as a risk factor, clinical implications for pre-operative testing, and study strengths/limitations.