-
Definition: PHOMS are oval, hyperreflective structures visualized on OCT B-scans around the optic nerve head, considered a marker of axoplasmic stasis.
-
Prevalence: Found in 7% of eyes across a broad spectrum of neurologic disorders; higher prevalence (up to 44% in intracranial hypertension [IH]) compared to 3-4% in healthy controls.
-
Associated Conditions:
-
Neuroimmunologic diseases (NID) (e.g., multiple sclerosis, neuromyelitis optica spectrum disorders): 4% prevalence.
-
Epilepsy: 7% prevalence.
-
Movement disorders (MD): 6% prevalence.
-
Intracranial hypertension (IH): 44% prevalence, strongly associated with increased intracranial pressure (ICP).
-
Inborn errors of metabolism (IEM): 9% prevalence.
-
-
Localization: Predominantly nasal (>65%), with minimal temporal involvement (5-10%); exclusively temporal PHOMS reported in Leber’s hereditary optic neuropathy.
-
Volume:
-
Median PHOMS volume: 0.06 mm³.
-
Significantly larger in IH (median 0.23 mm³) compared to NID (0.03 mm³), epilepsy (0.05 mm³), and MD (0.02 mm³).
-
Larger volumes in IH suggest a link to elevated ICP.
-
-
Intensity: Comparable to optic nerve intensity (0.99 ± 0.19), lower than retinal layers, higher than outer nuclear layer; no significant intensity differences across cohorts.
-
Correlations:
-
Positive correlation with peripapillary retinal nerve fiber layer (pRNFL) thickness (global, nasal-inferior, temporal-inferior, temporal segments).
-
Positive correlation with Bruch membrane opening minimum rim width (BMO MRW), likely due to peripapillary retinal layer deflection.
-
Negative correlation with age (excluding IH patients), suggesting larger PHOMS in younger patients.
-
No correlation with body mass index (BMI) or BMO surface area.
-
-
Pathophysiology Hypotheses:
-
Axoplasmic stasis (supported by histopathologic findings in papilledema).
-
Impairment of glymphatic drainage or translaminar pressure gradient.
-
-
Diagnostic Importance: PHOMS are a non-specific marker but more frequent in neurologic disorders; must differentiate from optic disc drusen or papilledema.
-
Clinical Pearl: Larger PHOMS volumes in IH are a key exam question; consider PHOMS in OCT interpretation for neurologic patients to avoid misdiagnosis.
-
Research Implications: PHOMS presence impacts OCT parameters (e.g., pRNFL, BMO MRW), requiring consideration in non-ophthalmic neurologic studies.
-
Limitations: Cross-sectional study design and cohort heterogeneity (age, disease duration) limit conclusions on causality or disease-specific mechanisms.
Citation
Gemert JA, Christmann T, Kaufmann E, et al. Characterization of Peripapillary Hyperreflective Ovoid Mass-like Structures in a Broad Spectrum of Neurologic Disorders. Ophthalmology. 2025;132(5):590-597. https://doi.org/10.1016/j.ophtha.2024.12.013
Intrapapillary Hemorrhage with Adjacent Peripapillary Subretinal Hemorrhage (IHAPSH)
General Overview
-
IHAPSH is an increasingly recognized condition, often associated with myopia-related optic disc changes.
-
Typically presents in young adults and school-aged children, particularly in East Asian populations.
-
Spontaneous resolution of hemorrhages and optic disc swelling is common without treatment.
-
Strong association with myopia, suggesting structural optic nerve head abnormalities as a primary cause.
Clinical Presentation
-
Age at onset: 12–30 years (mean 18.6 years).
-
Sex distribution: Predominantly female (4:1 female-to-male ratio).
-
Affected eyes: Unilateral (most cases), with rare bilateral involvement.
-
Refractive error: Myopic, ranging from -1.75 to -7.00 D (mean -5.38 D).
-
Axial length: 24.73–27.34 mm (mean 26.30 mm).
-
Visual function: Mild impairment, with normal best-corrected visual acuity (BCVA) (e.g., 20/16) and no significant color vision or light reflex abnormalities.
-
Visual field defects: Mariotte’s blind spot enlargement or decreased lower visual field sensitivity in some cases, often resolving with hemorrhage.
-
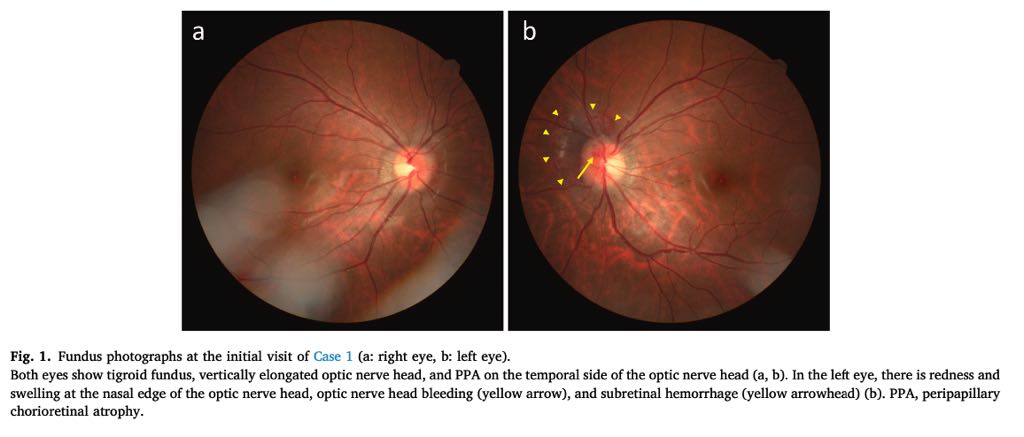
Funduscopic findings:
-
Crescent-shaped subretinal hemorrhage adjacent to the nasal superior optic disc.
-
Optic disc hemorrhage and swelling.
-
Vitreous hemorrhage in some cases (3/6 eyes).
-
Peripapillary chorioretinal atrophy (PPA) in all cases.
-
-
Associated optic disc abnormalities:
-
Optic disc drusen, tilted disc, small disc, or superior segmental optic hypoplasia (SSOH).
-
-
Systemic history: No significant systemic diseases or trauma; one case linked to exercise (running).
Diagnostic Imaging
-
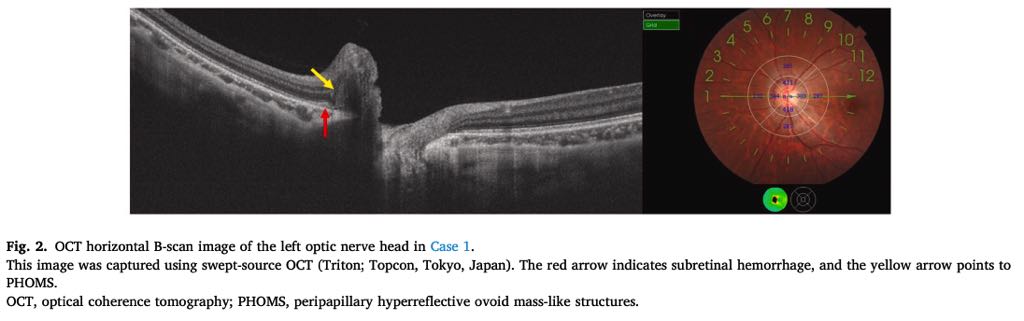
Optical Coherence Tomography (OCT):
-
Peripapillary hyperreflective ovoid mass-like structures (PHOMS) observed in all cases, located above Bruch’s membrane.
-
Optic disc drusen identified as low-reflective structures within the optic disc.
-
Subretinal hemorrhage visible on B-scans.
-
Affected optic nerve head shows a narrower and deeper cup compared to the contralateral eye.
-
Larger tilt angle in affected eyes.
-
-
OCT Angiography (OCTA): No significant abnormalities reported in most cases.
-
Fundus Autofluorescence:
-
Hyperfluorescence within the optic disc, indicative of optic disc drusen.
-
-
Fluorescein Angiography:
-
Hyperfluorescence at the nasal edge of the optic nerve head, suggestive of tissue staining.
-
-
Fundus Photography:
-
Documents optic disc hemorrhage, subretinal hemorrhage, and optic disc abnormalities (e.g., SSOH, PPA).
-
Pathophysiology and Risk Factors
-
Myopia-related structural abnormalities of the optic nerve head are a primary cause.
-
Weak adhesion between retinal layers in myopic eyes increases hemorrhage risk.
-
Optic disc abnormalities (small disc, tilted disc, optic disc drusen) may cause compression or circulation disturbances, predisposing to IHAPSH.
-
PHOMS:
-
Not specific to IHAPSH; also seen in pseudopapilledema, choked disc, anterior ischemic optic neuropathy, central retinal vein occlusion, and optic neuritis.
-
Associated with myopia, tilted discs, and smaller Bruch’s membrane opening.
-
Prevalence: 8.9% in healthy children aged 11–12 years.
-
-
Social factors: Increased tablet computer use among children may contribute to myopia progression and IHAPSH incidence.
Management and Prognosis
-
No treatment required: Hemorrhages and optic disc swelling resolve spontaneously within ~1 month.
-
No recurrence observed in affected eyes, and no onset in contralateral eyes in the study.
-
Monitoring:
-
Regular fundus examination and OCT to confirm resolution.
-
Visual field testing to assess Mariotte’s blind spot or sensitivity changes.
-
-
Long-term follow-up needed to understand IHAPSH’s relation to myopic optic neuropathy.
Epidemiology
-
Predominantly reported in East Asian populations.
-
Increasing incidence in Japan, possibly linked to myopia progression in younger populations.
-
Associated with axial length elongation during childhood and young adulthood.
Citation
-
Takemoto D, Ohkubo S, Udagawa S, Higashide T. Clinical presentation and optical coherence tomography findings of intrapapillary hemorrhage with adjacent peripapillary subretinal hemorrhage. Am J Ophthalmol Case Rep. 2025;38:102329. Available at: www.ajocasereports.com.