Factors Associated with Retinal Detachment Following Pediatric Cataract Surgery in the IRIS® Registry
– Study Overview:
– Retrospective cohort study using the IRIS® Registry (2013–2020) to identify risk factors for retinal detachment (RD) after pediatric cataract surgery in children <18 years.
– Purpose: To analyze predictors of RD diagnosis and repair within 5 years post-surgery, leveraging a large, diverse dataset including privately and publicly insured patients.
– Study Population:
– Included 7,407 children (53% male, 49% White non-Hispanic, median age 11.0 years) undergoing cataract surgery.
– Exclusions: Prior RD (exudative, tractional, rhegmatogenous), stage 4/5 retinopathy of prematurity (ROP), or unknown cataract laterality.
– Median follow-up: 1.6 years (IQR 0.4–3.6 years).
– Methodology:
– Cataract surgery identified via CPT codes; RD diagnosis and repair via ICD-9/10 and CPT codes.
– Data collected: Demographics (age, sex, race/ethnicity, insurance, region), clinical factors (ocular trauma, aphakia, premature retina [stage 0–3 ROP], persistent fetal vasculature [PFV], degenerative high myopia, lens subluxation).
– Statistical analysis:
– Kaplan-Meier estimator for 5-year cumulative incidence of RD diagnosis and repair.
– Multivariable Cox regression for hazard ratios (HRs), adjusting for all demographic and clinical factors.
– P<0.05 for significance; multicollinearity checked via variance inflation factor.
– Key Findings:
– Cumulative incidence (5 years post-surgery):
– RD diagnosis: 3.8% (95% CI 3.1–4.5%, 168 cases).
– RD repair: 1.6% (95% CI 1.2–2.0%, 76 cases).
– Significant risk factors for RD diagnosis:
– Ocular trauma (HR 2.22, 95% CI 1.39–3.57, P<0.001).
– Aphakia (HR 2.10, 95% CI 1.43–3.10, P<0.001).
– Premature retina (stage 0–3 ROP) (HR 2.73, 95% CI 1.36–5.48, P=0.005).
– Persistent fetal vasculature (PFV) (HR 3.26, 95% CI 1.58–6.71, P=0.001).
– Hispanic ethnicity (HR 1.71, 95% CI 1.15–2.54, P=0.008).
– Significant risk factors for RD repair:
– Aphakia (HR 3.98, 95% CI 2.33–6.79, P<0.001).
– Ocular trauma (HR 2.24, 95% CI 1.17–4.30, P=0.015).
– PFV (HR 5.47, 95% CI 1.85–16.2, P=0.002).
– Hispanic ethnicity (HR 2.71, 95% CI 1.54–4.78, P<0.001).
– Non-significant factors:
– Degenerative high myopia (HR 1.31, P=0.499 for diagnosis; HR 1.84, P=0.206 for repair).
– Lens subluxation (HR 1.56, P=0.176 for diagnosis; HR 1.85, P=0.131 for repair).
– Sex, age (though younger age [0–6 years] had lower HR vs. 7–18 years), region, insurance type.
– Timing:
– Median time to RD diagnosis: 4.4 months (IQR 0.8–13.4); shorter with trauma (1.2 months vs. 5.6 months, P=0.007).
– Median time to RD repair: 3.1 months (IQR 0.7–8.8).
– RD events peaked within first year post-surgery.
– Clinical Implications:
– High-risk groups (trauma, aphakia, PFV, premature retina, Hispanic ethnicity) require closer postoperative monitoring (e.g., dilated fundus exams) to detect RD early.
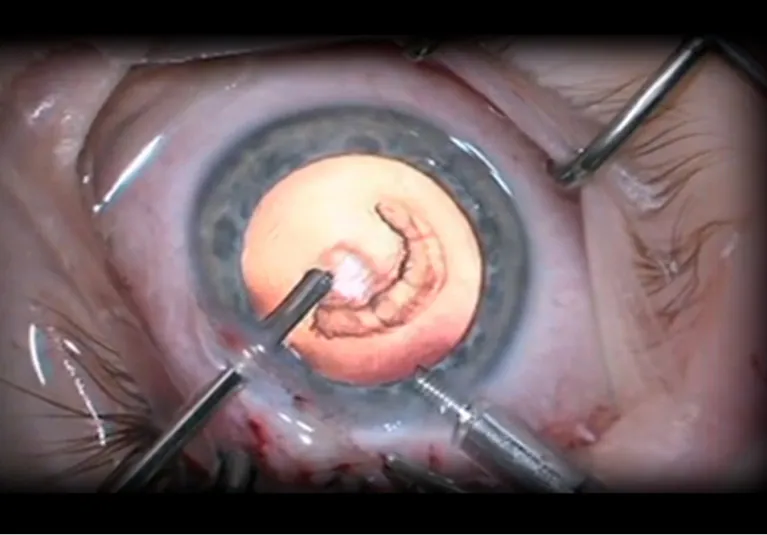
– Aphakia increases RD risk due to vitreoretinal traction from anterior vitrectomy and adherent pediatric vitreous, informing IOL vs. aphakia decisions in younger patients.
– Trauma underscores need for long-term surveillance, as RD may develop months/years later due to proliferative vitreoretinopathy (PVR) or delayed vitreous degeneration.
– Hispanic ethnicity association suggests potential socioeconomic barriers (e.g., limited prior eye care, higher trauma risk), warranting targeted follow-up strategies.
– Findings guide preoperative counseling on RD risk and surgical planning to minimize vitreoretinal disruption.
– Pathophysiology Context:
– Aphakia: Limited anterior vitrectomy in pediatric eyes (with adherent posterior hyaloid) increases risk of retinal breaks and traction, leading to RD.
– Ocular trauma: Causes mechanical retinal disruption, PVR, or delayed subretinal fluid accumulation, exacerbated in growing eyes.
– PFV: Associated with retinal structural abnormalities, increasing RD susceptibility.
– Premature retina: Altered retinal development (stage 0–3 ROP) predisposes to RD, though less severe than stage 4/5 ROP (excluded).
– Hispanic ethnicity: May reflect environmental/socioeconomic factors (e.g., trauma exposure, access to care) rather than genetic predisposition.
– Comparison to Prior Literature:
– Incidence: 3.8% RD diagnosis rate aligns with prior studies (0.8–15.2%), though variability due to cohort differences (e.g., Oke et al. reported similar risks using claims data).
– Risk factors: Consistent with prior findings on trauma, aphakia, and PFV (e.g., Agarkar et al., Haargaard et al.); premature retina less studied but significant here.
– Hispanic ethnicity: Novel finding, not reported in prior studies, possibly due to IRIS Registry’s diverse cohort.
– High myopia: No significant association contrasts with Rabiah et al., likely due to focus on degenerative high myopia (harder to diagnose in young children without axial length data).
– Sex: No male predominance, unlike some studies linking male sex to trauma-related RD, suggesting nuanced risk factors in this cohort.
– Strengths:
– Largest cohort to date (n=7,407), enabling analysis of rare outcomes like RD.
– IRIS Registry diversity: Includes privately/publicly insured children, enhancing generalizability vs. claims-based studies.
– Multivariable adjustment for confounders (e.g., trauma, aphakia, ethnicity).
– Robust statistical methods (Kaplan-Meier, Cox regression) with clear outcome definitions (diagnosis vs. repair).
– Limitations:
– Coding errors: Potential miscoding/under-coding of diagnoses (e.g., PFV, unspecified RD subtypes) may affect accuracy.
– Selection bias: Underrepresentation of academic centers in IRIS Registry.
– Missing data: No intraoperative complication details (e.g., capsule tears, zonulolysis), visual acuity, or systemic factors (e.g., developmental delays).
– Follow-up variability: Median 1.6 years, with potential loss to follow-up underestimating long-term RD risk.
– Hispanic ethnicity: Association may reflect socioeconomic confounders not fully captured (e.g., access to care).
These points emphasize RD incidence (3.8%), key risk factors (trauma, aphakia, PFV, premature retina, Hispanic ethnicity), clinical need for vigilant monitoring, and study strengths/limitations.