Aflibercept With vs Without Reduced-Fluence Photodynamic Therapy for Polypoidal Choroidal Vasculopathy
– Study Overview:
– Double-masked, sham-controlled, randomized clinical trial conducted at 2 centers in Singapore (January 2021–June 2024) to compare reduced-fluence photodynamic therapy (RF-PDT) + intravitreal aflibercept injection (IAI) vs IAI monotherapy in polypoidal choroidal vasculopathy (PCV).
– Objective: Assess functional (visual acuity) and anatomical (polyp closure) outcomes in PCV, a subtype of neovascular age-related macular degeneration (nAMD) prevalent in Asian populations (up to 50% vs 20% in Caucasians).
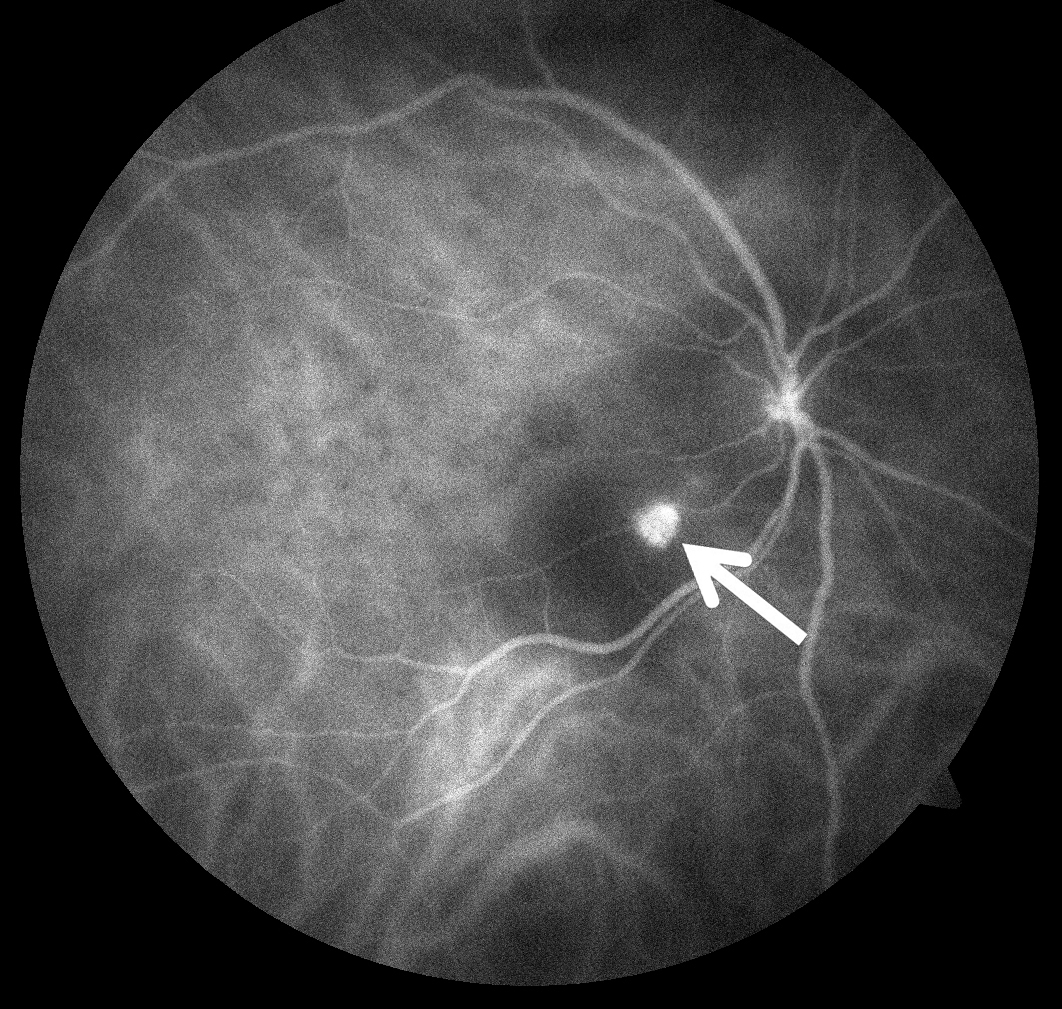
– PCV characteristics: Polypoidal lesions (PL) and branching vascular network (BVN) on indocyanine green angiography (ICGA), causing vision loss via exudation or hemorrhage, risking scarring or macular atrophy.
– Study Population:
– Included 60 participants (43 male [71.6%], mean age 71.3 years, mostly Chinese [90%]) aged ≥50 with symptomatic macular PCV confirmed by ICGA.
– Enrollment shortfall: Only 60 of planned 160 enrolled due to COVID-19 delays and verteporfin shortages, limiting statistical power.
– Baseline BCVA: 62.0 letters (Snellen ~20/63) in both arms; central subfield thickness (CST): 358 µm (combination) vs 435 µm (monotherapy).
– 100% follow-up at 52 weeks, with no dropouts.
– Interventions:
– Randomization (1:1):
– Combination arm: Single RF-PDT (25 J/cm², 689 nm, targeting PL and BVN) + 2 mg IAI at baseline.
– Monotherapy arm: Sham PDT (0 fluence) + 2 mg IAI at baseline.
– Follow-up: Monthly assessments (weeks 4–52) with pro re nata (PRN) IAI retreatment based on protocol criteria (e.g., persistent fluid, vision loss).
– RF-PDT rationale: Reduced fluence to minimize acute exudation risk seen with full-fluence PDT (50 J/cm²), supported by animal models showing similar choroidal neovascularization closure rates at half-fluence.
– Outcomes:
– Primary outcome: Mean change in best-corrected visual acuity (BCVA) from baseline to week 52.
– Result: Combination: +12.7 letters; Monotherapy: +11.9 letters; difference: 0.8 letters (95% CI, -3.0 to 6.0; P=.82).
– Interpretation: No superiority detected for either arm; combination not proven noninferior (within 5-letter margin) due to underpowered sample.
– Key secondary outcome: PL closure rate at week 12 (ICGA).
– Result: Combination: 20/30 (66.7%); Monotherapy: 10/30 (33.3%); difference: 33.4% (95% CI, 9.5–57.2%; P=.02).
– Caveat: Not adjusted for multiple analyses, considered hypothesis-generating, not clinically significant for functional outcomes.
– Other secondary outcomes (week 52, unadjusted):
– PL closure: 73.3% (combination) vs 46.7% (monotherapy) (P=.06).
– CST change: -119.8 µm (combination) vs -152.0 µm (monotherapy) (P=.11).
– Injection frequency: Mean 5.2 (combination) vs 5.7 (monotherapy) (P=.28), no significant reduction with PDT.
– Fluid presence: Subretinal fluid (SRF) in 26.7% (combination) vs 36.7% (monotherapy); intraretinal fluid (IRF) in 10% vs 13.3% (non-significant).
– Adverse events: No severe ocular events (e.g., endophthalmitis, retinal detachment); mild events (e.g., conjunctival hemorrhage) similar between arms.
– Clinical Implications:
– BCVA equivalence: IAI monotherapy achieves comparable visual gains to combination therapy, supporting its use as a first-line treatment for PCV.
– PL closure: Higher early closure with RF-PDT + IAI suggests potential anatomical benefit, but no functional advantage at 52 weeks, questioning routine PDT use.
– Injection burden: No reduction with combination therapy in PRN regimen, unlike hypotheses from EVEREST II (full-fluence PDT + ranibizumab, fewer injections).
– RF-PDT role: May be considered for refractory cases (persistent PL activity despite IAI), pending further studies, but not standard due to cost and access issues.
– Patient counseling: Emphasize IAI efficacy; discuss PDT for anatomical goals only if monotherapy response is inadequate.
– Pathophysiology Context:
– PCV: PLs are primary hemorrhage sources, targeted by PDT for closure; anti-VEGF (IAI) addresses exudation from PL and BVN.
– PDT mechanism: Verteporfin-activated laser induces thrombosis in PL, reducing leakage, but risks choriocapillaris damage or atrophy with repeated sessions.
– RF-PDT: Aims to balance efficacy and safety, though comparative data vs full-fluence PDT are lacking.
– Comparison to Prior Studies:
– EVEREST II (ranibizumab + full-fluence PDT vs ranibizumab):
– Superior BCVA gain (8.3 vs 5.1 letters) and PL closure (69.3% vs 34.7%) at 12 months with combination; no BCVA difference at 6 years.
– Fewer injections with PDT (driven by fixed dosing in monotherapy).
– Contrast: Current study used aflibercept, RF-PDT, and PRN dosing, with no BCVA or injection benefit.
– PLANET (aflibercept ± rescue PDT):
– IAI monotherapy achieved good BCVA (+10.7 letters) and PL inactivation, but low PL closure (<50%).
– Only 15% needed rescue PDT, limiting combination insights.
– Current study: Higher PL closure with upfront PDT, but no functional gain.
– PL closure rates: Current study’s 73.3% (combination, week 52) compares to EVEREST II’s 69.3%, suggesting RF-PDT may be effective, though not directly compared.
– Strengths:
– Prospective RCT with double-masking and comprehensive imaging (ICGA, OCT, fluorescein angiography).
– Novel design: First to evaluate RF-PDT + IAI vs IAI in PCV with PRN regimen, addressing gaps from PLANET (fixed dosing, rescue PDT).
– Complete follow-up: 100% retention enhances data reliability.
– Real-world relevance: PRN dosing mirrors clinical practice.
– Limitations:
– Underpowered: Only 37.5% of planned sample (60/160), reducing ability to detect BCVA differences or confirm noninferiority.
– Short follow-up: 52 weeks insufficient to assess long-term outcomes (e.g., atrophy, recurrence).
– Single PDT session: Limits evaluation of repeated PDT effects; EVEREST II allowed multiple sessions.
– RF-PDT uncertainty: No direct comparison to full-fluence PDT, unclear if fluence reduction impacts efficacy.
– Secondary outcomes: Unadjusted P-values (e.g., PL closure) risk type I error, requiring cautious interpretation.
– Generalizability: Predominantly Chinese cohort may not fully apply to other ethnicities (e.g., Caucasians with lower PCV prevalence).
These points emphasize no BCVA benefit of RF-PDT + IAI, higher early PL closure as hypothesis-generating, IAI monotherapy efficacy, and study limitations (underpowered, short follow-up).