Retina and Uveitis MCQs – part 1
QUESTIONS
۱–۴
A 45-year-old male complains of slowly progressive decreased vision in his left eye for 2 months. Visual acuity is 20/200. His fundus examination and OCT are shown in Figures 12-1A and B.
FIGURE 12-1A–B
۱ Which of the following best represents the pathophysiology of this patient’s condition?
A) Embolic phenomenon
B) Thrombosis at the level of the lamina cribrosa
C) Carotid stenosis
D) Compression of the central retinal vein due to an atherosclerotic arteriole
۲ All of the following would be acceptable in the management of this patient except:
A) dexamethasone intravitreal implant (Ozurdex™)
B) vitrectomy with sheathotomy
C) intravitreal anti-VEGF agent
D) gonioscopy
۳ Which of the following is the most serious vision-threatening complication of this condition?
A) Cataract progression
B) Retinal detachment
C) Rubeosisiridis with secondary neovascular glaucoma
D) Refractive shift
۴ All of the following systemic conditions may be associated with this condition, except:
A) hypertension
B) protein C/S deficiency
C) abnormal serum electrophoresis
D) low serum homocysteine
۱ B) Thrombosis at the level of the lamina cribrosa
Figure 12-1A shows the classic appearance of a CRVO with dilated and tortuous retinal vasculature coupled with four quadrants of intraretinal hemorrhages.
The pathophysiology of CRVO is due to thrombosis at the level of the lamina cribrosa. In contrast, compression of a retinal vein by a retinal arteriole is the pathophysiology of a branch retinal vein occlusion (BRVO, choice D), not CRVO.
Embolic phenomena are more likely to cause arterial occlusions such as BRAO and/or CRAO stemming from the carotid artery or heart.
Carotid stenosis may give a similar appearance to CRVO; however, it more likely may result in the ocular ischemia syndrome (OIS), in which the fundus appearance has dilated, but not tortuous retinal vasculature, and there tend to be smaller, more mid–peripheral retinal hemorrhages.
۲ B) Vitrectomy with sheathotomy
The initial management of a CRVO should include gonioscopy to exclude the presence of neovascularization of the angle (NVA), which may indicate neovacular glaucoma (NVG).
Based on the GENEVA Study, the dexamethasone intravitreal implant is FDA-approved for the treatment of macular edema secondary to CRVO. Complications of intravitreal steroids include cataract progression and raised intraocular pressure. Based on the CRUISE Study, intravitreal ranibizumab is FDA-approved for the treatment of macular edema secondary to CRVO.
۳ C) Rubeosisiridis with secondary neovascular glaucoma
Rubeosis and secondary neovascular glaucoma may result in irreversible optic nerve damage and severe vision loss. Therefore, prompt treatment with ocular antihypertensives and possibly filtration surgery may be required for glaucoma management. The underlying cause of the rubeosis must be treated with prompt PRP. Fortunately, in the era of anti-VEGF agents, this sight-threatening complication is less frequently encountered.
۴ D) Low serum homocysteine
The majority of CRVOs are associated with hypertension. However, in the younger population, a secondary systemic etiology may be the cause such as protein C/S deficiency, or elevated (not low) serum homocysteine, or a hyperviscosity syndrome such as multiple myeloma or Waldenstrom’s.
۵
A 36-year-old asymptomatic male is referred by his optometrist for the following ocular findings (Fig. 12-2). All of the following historical facts may be pertinent in determining the underlying diagnosis except:
FIGURE 12-2
A) history of liver transplantation
B) history of multiple, nonspecific episodes of weakness and numbness
C) history of high-risk sexual behavior
D) history of polydipsia, polyphagia, polyuria
Figure 12-2 shows the appearance of multiple peripapillary cotton-wool spots in an asymptomatic patient that are characteristic of interferon retinopathy. Interferon is a medication often used in patients with a history of liver transplantation (choice A).
Fundus photographs of both eyes at presentation, demonstrating multiple peripapillary cotton-wool spots bilaterally
Although the differential diagnosis of cotton-wool spots is large, the most common etiologies include diabetes (choice D), and hypertension. Other causes of this appearance would include HIV (choice C). Choice B refers to a patient with multiple sclerosis, who would not be expected to have this fundus appearance. Patients with MS may develop optic neuritis and/or intermediate uveitis.
۵ B) History of multiple, nonspecific episodes of weakness and numbness
QUESTIONS
۶ and 7
A 73-year-old female with a history of well-controlled diabetes recently underwent uncomplicated phacoemulsification with a posterior chamber intraocular lens and complains of blurry vision. Best-corrected visual acuity (BCVA) is 20/60. Her fluorescein angiogram and OCT are provided in Figure 12-3.
FIGURE 12-3
۶ Which retinal layer accounts for the appearance of this patient’s vision loss?
A) Nerve fiber layer
B) Outer plexiform
C) Inner plexiform
D) Outer nuclear
۷ All of the following are acceptable treatment options for this patient’s vision loss except:
A) topical prednisolone
B) topical NSAID
C) focal grid laser
D) observation
۶ B) Outer plexiform
Figure 12-3 shows a fluorescein angiogram of classic petalloid hyperfluorescence. The “petalloid” leakage pattern on IVFA is due the accumulation of serous fluid in the outer plexiform layer of the retina, which is seen on the spectral-domain OCT image.
۷ C) Focal grid laser
Approximately ۱% of patients undergoing routine phacoemulsification may develop the Irvine–Gass syndrome, or postcataract CME. The natural history of untreated CME is quite good, but may take up to 6 to 9 months. Generally accepted methods of treatment include observation, topical steroids, and/or topical NSAIDs.
Focal grid laser would not be indicated in this setting, unless there was concominant diabetic macular edema with leaking microaneursyms on IVFA.
QUESTIONS
۸–۱۱
A 73-year-old Caucasian female complains of sudden, painless vision loss in her left eye. BCVA measures 20/20 in her right eye and ۲۰/۶۰ in her left eye. Her fundus photos and early and late fluorescein angiogram are provided in Figure 12-4A. The OCT of her left eye is provided in Figure 12-4B.
FIGURE 12-4A–B
۸ All of the following are FDA-approved for the treatment of her condition except:
A) intravitreal bevaziumab (Avastin™)
B) intravitreal ranibizumab (Lucentis™)
C) intravitreal aflibercept (Eylea™)
D) intravenous verteporfin (Visudyne™)
۹ According to the Comparison of Age-Related Macular Degeneration Treatments Trial (CATT), which of the following is true?
A) Intravitreal bevacizumab is superior to ranibizumab
B) Intravitreal ranibizumab is superior to bevacizumab
C) Intravitreal bevacizumab is safer than ranibizumab
D) Intravitreal bevacizumab is noninferior to ranibizumab
۱۰ What is the approximate incidence of postintravitreal injection endophthalmitis?
A) ۱ in 7,500
B) ۱ in 2,500
C) ۱ in 10,000
D) ۱ in 5,000
۱۱ According to the ANCHOR clinical trial regarding the use of intravitreal ranibizumab for neovascluar age-related macular degeneration (ARMD), approximately what percent of patients gain at least three lines of vision after 2 years of therapy?
A) ۱۰%
B) ۵۰%
C) ۹۰%
D) ۳۰%
۸ A) Intravitreal bevacizumab (Avastin™)
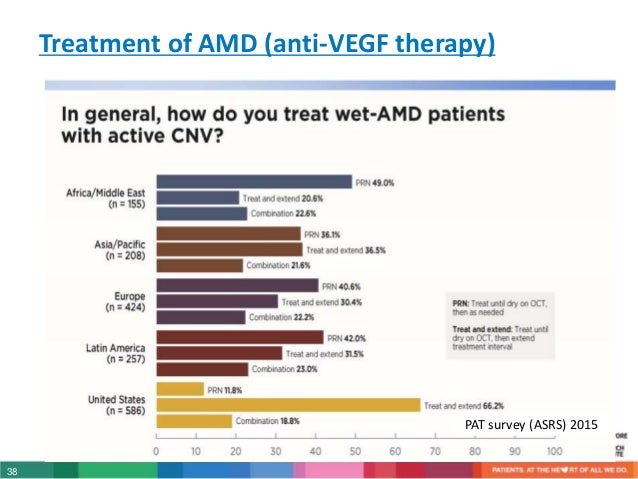
The treatment of neovascular (wet) ARMD has revolutionized with the advent of intravitreal anti-VEGF agents. As of 2013, both intravitreal ranibizumab (Lucentis™, Genentech, South San Francisco) and aflibercept (Eylea™, Regeneron, NY) are FDA-approved for the treatment of neovascular ARMD.
Visudyne™ (photodynamic therapy, PDT) is an older treatment modality that is FDA-approved for the treatment of wet ARMD, but was shown to have inferior visual outcomes compared to intravitreal ranibizumab in the ANCHOR study.
According the PAT survey in 2012, approximately ۶۷% of retina specialists in the United States use intraviteral bevacizumab off-label as first-line treatment of wet ARMD.
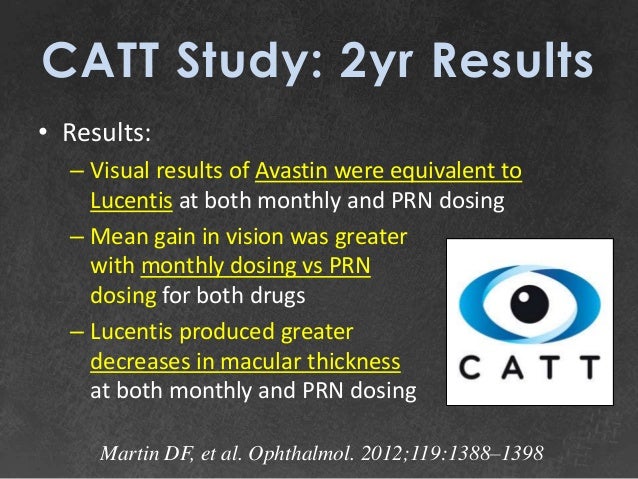
۹ D) Intravitreal bevacizumab is noninferior to ranibizumab.
The CATT was a large, prospective, multicenter, randomized, noninferiority clinical trial comparing intravitreal bevacizumab and ranibizumab for the treatment of neovascular ARMD. At the end of 2 years of treatment, bevacizumab was shown to be noninferior to ranibizumab.
The study was not designed to determine any differences in the safety between the two medicines.
۱۰ B) 1 in 2,500
The reported incidence of endophthalmitis following intravitreal injection of anti-VEGF agents is between 1 in 2,000 and 1 in 3,000.
۱۱ D) 30%
The anti-vascular endothelial growth factor antibody for the treatment of predominately classic choroidal neovacularization in Age-related Macular Degeneration (ANCHOR) Trial was a prospective, randomized clinical trial that compared intravitreal ranibizumab with verteporfin PDT for neovacular ARMD. At the end of 2 years of treatment, approximately 30% of patients treated with ranibizumab gained at least three lines of vision and 90% of patients lost less than three lines of vision.
۱۲
A 33-year-old female complains of bilateral vision loss for 4 months. Visual acuity measures CF and 20/100. Her fundus photos are provided in Figure 12-5. All of the following may be associated with the development of this condition except:
FIGURE 12-5
A) disseminated intravascular coagulation
B) polyarteritisnodosa
C) retinitis pigmentosa (RP)
D) toxemia of pregnancy
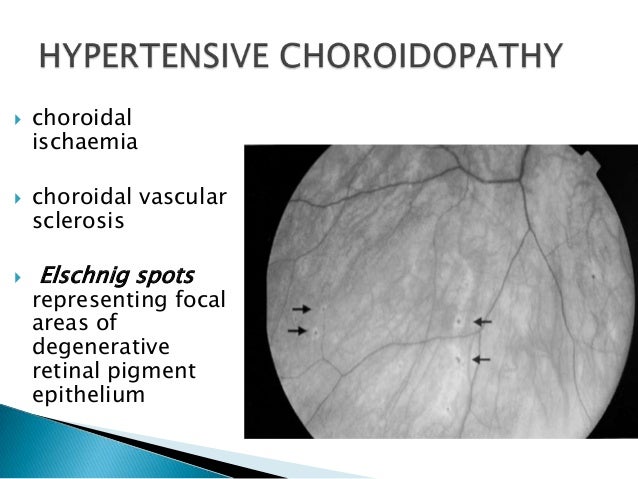
Figure 12-5 shows the classic fundus appearance of choroidal infarcts that leave wedge-shaped hyperpigmented areas in the fundus. The wedge-shaped defects are thought to follow the lobular anatomy of the choroidal blood flow.
The differential diagnosis of choroidal infarction includes accelerated (malignant) hypertension, such as from toxemia of pregnancy. Other causes include disseminated intravascular coagulation, and inflammatory conditions such as polyarteritis nodosa.
Hypertensive chorioretinopathy with Elschnig spots :
Photographs of right (a) and left (b) fundi at 3 weeks after presentation, showing bilateral optic disc oedema, subretinal exudation, right subfoveal scarring, left macular star exudate configuration, and Elschnig spots. Photographs of right (c) and left (d) fundi at 4 months after presentation and treatment, showing resolution of disc oedema, resorption of exudate, as well as residual Elschnig spots and peripapillary pigmentation. Elschnig spots in the mid-periphery, seen at 3 weeks (e) and 4 months (f) after presentation.
The appearance of RP typically causes perivascular RPE hyperpigmentation, termed “bone-spicules” with vascular attenuation, and waxy pallor of the optic nerve.
so the correct answer is C) Retinitis pigmentosa (RP) .
QUESTIONS
۱۳–۱۷
Match the following descriptions of the retinal layers with their corresponding labeled spectral-domain OCT layers on Figure 12-6.
FIGURE 12-6
۱۳ This layer represents the junction between the photoreceptor inner and outer segments:
A) Z
B) X
C) V
D) W
۱۴ A cotton-wool spot represents an infarct of this layer:
A) X
B) Y
C) V
D) Z
۱۵ This layer is responsible for the major source of nutrition of the retinal pigment epithelium (RPE):
A) Z
B) W
C) V
D) Y
۱۶ This layer represents interconnections between photoreceptors, bipolar, and horizontal cells:
A) W
B) Y
C) W
D) Z
۱۷ The cell bodies in this layer have their axons in the nerve fiber layer:
A) W
B) V
C) Y
D) X
۱۳ B) X – IS–OS junction (ellipsoid layer)
۱۴ D) Z – nerve fiber layer
۱۵ C) V – choriocapillaris
۱۶ B) Y – outer plexiform layer
۱۷ A) W – ganglion cell layer
QUESTIONS
۱۸–۲۰
A 34-year-old white man reports that he has had floaters for 1 week. His fundus examination is shown in Figure 12-7.
FIGURE 12-7
۱۸ Which systemic condition is most relevant to the diagnosis?
A) Insulin-dependent diabetes mellitus since age 11
B) Uncontrolled hypertension
C) Recurrent pneumonia, weight loss, and vascular skin lesions
D) Sickle cell anemia
۱۹ Which of the following would be seen histopathologically?
A) Retinal necrosis
B) Loss of pericytes
C) Macroaneurysms
D) Thickening and excrescences on Bruch membrane
۲۰ What ocular complication may be associated with this condition?
A) Retinal detachment
B) Neovascular glaucoma
C) Neovascularization of the optic disc
D) Siegrist streaks
۱۸ C) Recurrent pneumonia, weight loss, and vascular skin lesions
The fundus photo in Figure 12-7 depicts multiple cotton-wool spots and hemorrhagic necrosis of the retina after a vascular distribution. In a young patient with recurrent infections, immune deficiency should be considered, and HIV status should always be ascertained.
From ۱۵% to 40% of patients with AIDS develop CMV retinitis. Common presenting symptoms include floaters and decreased vision. Cotton-wool spots and hemorrhages may be seen in branch retinal vein occlusions; however, there would be no associated vitritis.
۱۹ A) Retinal necrosis
CMV retinitis is a hemorrhagic necrotizing retinitis involving all retinal layers. Intranuclear inclusion bodies may be found. Loss of pericytes and macroaneurysms can be seen with diabetes. Thickening and excrescences of Bruch membrane correspond to the drusen seen in ARMD.
۲۰ A) Retinal detachment
CMV retinitis can lead to significant atrophy of the retina and subsequent retinal detachment. Oftentimes, multiple retinal defects are present, and the patients need long-term internal tamponade with silicone oil to prevent recurrent detachments.
Siegrist streaks are atrophic areas of the RPE overlying areas of infarction of a choroidal lobule and may be found with hypertensive retinopathy.
QUESTIONS
۲۱ and 22
A 60-year-old woman with diabetes mellitus and hypertension reports having difficulty reading for the past 4 months. Her visual acuity is ۲۰/۲۵. Her fundus photograph, fluorecein angiogram, and OCT are shown in Figure 12-8.
FIGURE 12-8
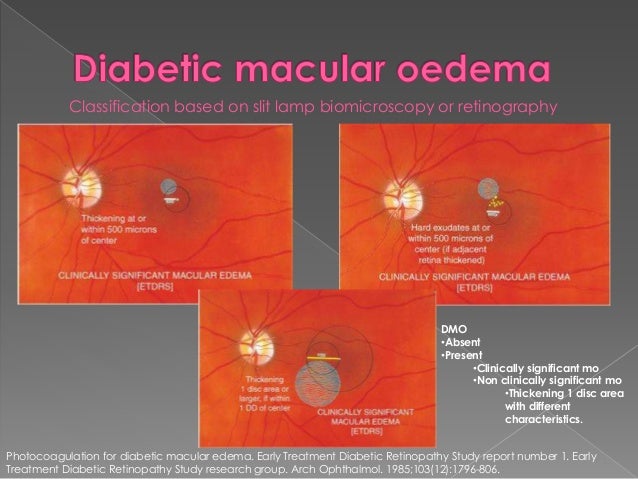
۲۱ According to the Early Treatment of Diabetic Retinopathy Study (ETDRS), which one of the following is considered clinically significant diabetic macular edema?
A) Hard exudates within 500 µm of the fovea
B) Retinal thickening greater than 1 disk area in size and within 1 disk diameter of the center of the fovea
C) Diffuse leakage on fluorescein angiography
D) A circinate ring of exudates located 2 disk areas from the fovea
۲۲ All of the following would be acceptable in the management of this patient except:
A) close observation with reevaluation in 2 months
B) intravitreal anti-VEGF agent
C) panretinal laser photocoagulation
D) focal laser photocoagulation
۲۱ B) Retinal thickening greater than 1 disk area in size and within 1 disk diameter of the center of the fovea
CSME is defined as one or more of the following criteria:
۱. Retinal thickening within 500 µm of the fovea.
۲. Hard exudates within 500 µm of the fovea with associated retinal thickening.
۳. Retinal thickening 1 disk area or greater, part of which is within 1 disk diameter of the fovea.
۲۲ C) Panretinal laser photocoagulation
This patient has diabetic macular edema, and at the current level of visual acuity of 20/25, close observation would be an acceptable management option, giving the patient the opportunity to work on his/her glycemic control.
Recently, based on the RISE/RIDE clinical trials, intravitreal ranibizumab ۰.۳ mg is FDA-approved for the treatment of diabetic macular edema. In the pooled data from these identical clinical trials, approximately ۴۰% of patients treated with ranibizumab versus 15% of patients treated with sham injection gained 15 letters after 2 years of treatment.
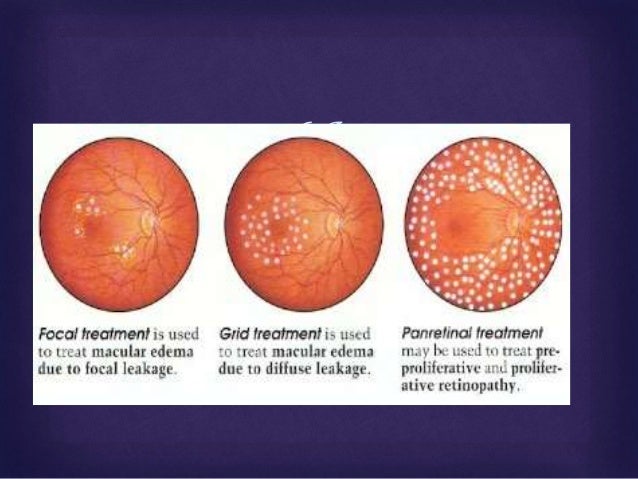
Based on the ETDRS, patients treated with focal laser photocoagulation had half the likelihood of moderate visual loss compared to untreated eyes. PRP is indicated for PDR and in fact may exacerbate macular edema.
QUESTIONS
۲۳–۲۵
A 7-year-old girl reports having poor vision for 2 weeks. She presents with a fundus as shown in Figure 12-9.
FIGURE 12-9
۲۳ What historical information might be helpful in the diagnosis?
A) Prematurity with low birth weight
B) Juvenile-onset diabetes mellitus
C) Blunt trauma to orbit with a soccer ball
D) A pet cat at home
۲۴ What laboratory studies are appropriate?
A) Urinalysis, stool for ova and parasites
B) Complete blood count (CBC), venereal disease research laboratories (VDRL) test, toxoplasma titer, viral titer screen, Bartonella IgG, and IgM
C) Antinuclear antibodies, serum protein electrophoresis (SPEP)
D) Lipoprotein, computed tomography (CT) of head and orbits
۲۵ What treatment would you offer?
A) Triple sulfa antibiotics
B) Vitrectomy
C) Observation
D) Laser photocoagulation
۲۳ D) A pet cat at home
The picture shown in Figure 12-9 and this history are suggestive of Leber idiopathic stellate neuroretinitis. The exact etiology of neuroretinitis is unknown but has been linked to viral infections (mumps, influenza, varicella) and other diseases (cat-scratch fever, leptospirosis).
۲۴ B) Complete blood count (CBC), venereal disease research laboratories (VDRL) test, toxoplasma titer, viral titer screen, Bartonella IgG, and IgM
Differential diagnosis may include syphilis, toxoplasmosis of the optic nerve, diffuse unilateral subacute neuroretinitis, trauma, systemic hypertension, and diabetes mellitus.
۲۵ C) Observation
The natural course of Leber stellate neuroretinitis is spontaneous resolution over several months. The prognosis is excellent, and over 80% of patients have visual acuity better than 20/40.
۲۶
Which one of the following about Coats disease is true?
A) Usually bilateral
B) Associated with microphthalmia
C) Bimodal age distribution
D) Equally common between males and females
Coats disease (congenital retinal telangiectasias) tends to occur unilaterally in otherwise healthy boys. The majority of boys have the juvenile form, with a peak incidence within the end of the first decade. An adult form occurs after age 16 and may be associated with hypercholesterolemia.
Correct answer :
C) Bimodal age distribution
AAO 2018 BCSC retina :
Coats Disease Coats disease is characterized by the presence of vascular dilatations (retinal telangiectasia), including ectatic arterioles, microaneurysms, venous dilations (phlebectasias), and fusiform capillary dilatations, which are frequently associated with exudative retinal detachment. Usually only 1 eye is involved, and there is a marked male predominance (۸۵%).
To date, researchers have not identified an associated gene or chromosome or any hereditary pattern, and no association between Coats disease and systemic disease has been found. In an eye with Coats disease, the abnormal vessels are compromised, resulting in the leakage of serum and other blood components, which accumulate in and under the retina. Any portion of the peripheral and macular capillary system may be involved. Although angiography demonstrates the presence of retinal capillary nonperfusion, posterior segment neovascularization is unusual.
The clinical findings vary widely, ranging from mild retinal vascular abnormalities and minimal exudation to extensive areas of retinal telangiectasia associated with massive leakage and exudative retinal detachment. The severity and rate of progression appear greater in children under the age of 4 years, in whom massive exudative retinal detachment with the retina apposed to the lens may simulate retinoblastoma or other causes of leukocoria (called Coats reaction; Fig 7-8; also see BCSC Section 6, Pediatric Ophthalmology and Strabismus, for the differential diagnosis of leukocoria) or xanthocoria (yellow pupil).
Patients with peripheral areas of leaky vascular anomalies typically present with lipid deposition in an otherwise angiographically normal macula, because “hard” exudate tends to accumulate in the macula. Similar findings in adults probably represent late decompensation of preexisting vascular anomalies.
Occasionally, the initial finding is a submacular lipogranuloma or subretinal fibrosis. The differential diagnosis for Coats disease may include dominant (familial) exudative vitreoretinopathy facioscapulohumeral muscular dystrophy retinopathy of prematurity (ROP) retinal hemangioblastomas (von Hippel–Lindau syndrome) For milder cases of lipid exudation, additional considerations are diabetic retinopathy, BRVO, juxtafoveal retinal telangiectasia, and radiation retinopathy.
Treatment of Coats disease generally consists of ablation with photocoagulation or cryotherapy, and, in severe cases, retinal reattachment surgery. Photocoagulation and cryotherapy are effective in obliterating the vascular anomalies and in halting progression. Several treatments may be necessary, and long-term follow-up is important to detect and treat recurrences or disease progression. Intravitreal anti–vascular endothelial growth factor (VEGF) therapy may be a useful adjunctive treatment that is resistant to ablative therapy alone.
۲۷
Which one of the following conditions has been associated with foveal hypoplasia?
A) Choroideremia
B) Aniridia
C) Juvenile X-linked retinoschisis (JXLR)
D) Tay–Sachs disease
Foveal hypoplasia has been associated with aniridia and albinism. Choroideremia shows a generalized choroidal dystrophy. Patients with JXLR may have foveal schisis, and Tay–Sachs disease may have a cherry red spot.
B) Aniridia
QUESTIONS
۲۸–۳۰
A 60-year-old white woman reports having poor vision in her left eye for 4 months. Her fundus photo and OCT are shown in Figure 12-10.
FIGURE 12-10
۲۸ What is her diagnosis?
A) Retinal detachment
B) Macular hole
C) Cystoid macular edema (CME)
D) Epiretinal membrane
۲۹ What would fluorescein angiography show?
A) Central hypofluorescence due to blockage
B) Leakage in petalloid pattern
C) Central window defect
D) Pooling of fluorescein
۳۰ What treatment might be offered?
A) Vitrectomy with intraocular gas injection
B) Laser photocoagulation
C) Sub-Tenon steroid injection
D) Scleral buckling procedure
۲۸ B) Macular hole
This patient has a stage IV macular hole. The borders of the macular hole may develop a cuff of subretinal fluid. Punctate yellow deposits may exist within the defect. Idiopathic macular holes are thought to arise from tangential traction on the foveal region by the posterior cortical vitreous.
۲۹ C) Central window defect
The RPE beneath the hole may undergo atrophy, leading to hyperfluorescence during choroidal filling on fluorescein angiography.
۳۰ A) Vitrectomy with intraocular gas injection
Pars plana vitrectomy with internal limiting membrane (ILM) peeling and intraocular gas injection is the preferred treatment for stage IV macular holes. With surgical intervention, patients may achieve over a 90% success rate of hole closure. Often, patients are instructed to maintain postoperative prone (facedown) positioning for 3 to 7 days; however, recent literature suggests that prone positioning may not be required for successful hole closure.
۳۱
All of the following are associated with the clinical finding shown in Figure 12-11 except:
FIGURE 12-11
A) vitreous hemorrhage (VH)
B) hypertension
C) renal cell carcinoma
D) macular edema
Figure 12-11 demonstrates a retinal arterial macroaneurysm. Macroaneurysms tend to occur in the elderly population and have been associated with systemic hypertension and atherosclerosis. Complications that may result include VH, macular edema, and exudates.
Renal cell carcinomas may be found in up to ۲۵% of patients with von Hippel–Lindau disease. These patients present with retinal hemangioblastomas rather than with macroaneurysms. Other systemic manifestations of this phakomatosis include pheochromocytomas, pancreatic and renal cysts, and hemangioblastomas of the CNS and visceral organs.
Fundoscopic photograph illustrating a retinal hemangioblastoma (arrows).
Retinal capillary hemangioblastoma (angiomatosis retinae, previously known as retinal capillary hemangioma) is a rare autosomal dominant condition with a reported incidence of 1 in 40,000. Typically, patients are diagnosed in the second to third decades of life, although retinal lesions may be present at birth. The retinal capillary hemangioblastoma appears as a red to orange tumor arising within the retina with large-caliber, tortuous afferent and efferent retinal blood vessels .
Associated yellow-white retinal and subretinal exudates that have a predilection for foveal involvement may appear. Exudative detachments often occur in eyes with hemangioblastomas. Atypical variations include hemangiomas arising from the optic disc, which may appear as encapsulated lesions with or without pseudopapilledema, and in the retinal periphery, where vitreous traction may elevate the tumor from the surface of the retina, giving the appearance of a free-floating vitreous mass.
Fluorescein angiography of retinal capillary hemangioblastomas demonstrates a rapid arteriovenous transit, with immediate filling of the feeding arteriole, subsequent filling of the numerous fine blood vessels that constitute the tumor, and drainage by the dilated venule.
Massive leakage of dye into the tumor and vitreous can occur.
When a capillary hemangioblastoma of the retina occurs as a solitary finding, the condition is generally known as von Hippel disease. This condition is familial in about 20% of cases and bilateral in about 50%. The lesions may be multiple in 1 or both eyes.
If retinal capillary hemangiomatosis is associated with a cerebellar hemangioblastoma, the term von Hippel–Lindau syndrome is applied. The gene for von Hippel–Lindau syndrome has been isolated on chromosome 3. A number of other tumors and cysts may occur in patients with von Hippel–Lindau syndrome. The most important of these lesions are cerebellar hemangioblastomas, renal cell carcinomas, and pheochromocytomas. Genetic screening now allows for subtyping of patients with von Hippel–Lindau to determine the risk for systemic manifestations of the disease. When this diagnosis is suspected, appropriate genetic consultation and screening are critical for long-term follow-up of ocular manifestations and the associated systemic complications. Screening for systemic vascular anomalies (eg, cerebellar hemangioblastomas) and malignancies (eg, renal cell carcinoma) may reduce mortality, while aggressive screening for and early treatment of retinal hemangioblastomas may reduce late complications of exudative detachment and improve long-term visual outcomes.
The treatment of retinal capillary hemangioblastomas includes photocoagulation for smaller lesions, cryotherapy for larger and more peripheral lesions, and scleral buckling with cryotherapy or penetrating diathermy for extremely large lesions with extensive retinal detachment. External-beam and charged-particle radiotherapy have also been used. More recently, PDT has been used successfully to treat retinal capillary hemangioblastomas.
Standard verteporfin dosing coupled with both standard and modified photodynamic protocols resulted in fibrosis of the hemangiomas with secondary retinal traction and improved visual acuity in recent studies.
Recent case reports have suggested the utility of targeted antiangiogenic therapy in the management of retinal capillary hemangioblastomas. The efficacy of antiangiogenic agents in the treatment of these vascular lesions is of compelling interest to von Hippel–Lindau patients, who have a lifelong risk of developing retinal angiomas. Both systemic and intravitreal VEGF inhibitors have been used.
Reports to date suggest that the principal efficacy of VEGF inhibitors is in reducing macular edema. The impact on the actual size of the hemangiomas has been variable. Thus, the visual prognosis remains guarded for patients with large retinal lesions.
so correct answer is
۳۱ C) Renal cell carcinoma