Laboratory Evaluation Of Hypercoagulable States In Patients With Central Retinal Vein Occlusion Who Are Less Than 56 Years Of Age
Purpose: To investigate whether the results of early tests for hypercoagulability are correlated with the development of central retinal vein occlusion risk factors later in life and to evaluate the necessity of these tests in younger patients.
Methods: This was a retrospective, observational case series. From January 1995 to December 2014, 55 patients aged below 56 years with central retinal vein occlusion (CRVO) were enrolled in the study.
Laboratory evaluations for homocysteine, activated protein C resistance, protein C activity, protein S activity, antithrombin III activity, antiphospholipid antibodies, and anticardiolipin antibodies were obtained at the onset of CRVO.
After 24 to 205 months, the presence of risk factors for CRVO such as hypertension, obesity, hyperlipidemia, diabetes mellitus, sleep apnea, and glaucoma was determined. Bilateral correlation and logistic regression were performed to determine the correlations between the results of the initial laboratory tests and the diagnosis of CRVO risk factors.
Results: The median follow-up was 168.5 months. Five patients completed at least 24nmonths of follow-up, 9 patients completed at least 5 years, and 36 patients completed at least 10 years. Five patients had no or less than 24 months’ follow-up. Fourteen of 50 patients (28%) had at least one positive test result at the onset of CRVO. At the end of follow-up, 11 patients had been diagnosed with obesity (22%), 29 with hypertension (58%), 21 with hyperlipidemia (42%), 24 with diabetes (8%), 5 with sleep apnea (10%), and 8 with glaucoma (16%). Among 36 patients with a minimum 10 years’ follow-up, 30 (83%) developed at least one common risk factor, and none experienced any thromboembolic events. There were no correlations between test results and the diagnosis of any risk factors in patients with a minimum of 2, 5, or 10 years’ follow-up (P . 0.05).
Conclusion: The results of laboratory tests evaluating hypercoagulability in young patients with CRVO are not correlated with later-developed commonly known risk factors. Many of the common risk factors were present by the end of the study, suggesting that they still remain the core etiology for the disease. The value of the thrombophilic tests is brought into question, as none of the patients demonstrated further clotting or any unusual thrombi with long-term follow-up. RETINA 0:1–۵, ۲۰۱۷
Checkpoint Inhibitor Immune Therapy Systemic Indications And Ophthalmic Side Effects
Purpose: To review immune checkpoint inhibitor indications and ophthalmic side
effects.
Methods: A literature review was performed using a PubMed search for publications between 1990 and 2017.
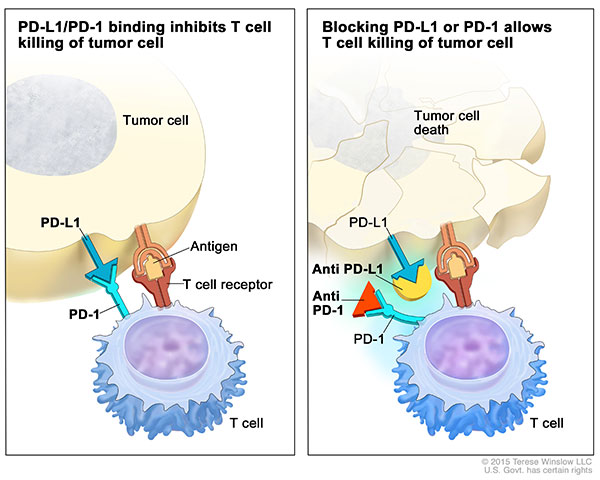
Results: Immune checkpoint inhibitors are designed to treat system malignancies by targeting one of three ligands, leading to T-cell activation for attack against malignant cells. These ligands (and targeted drug) include cytotoxic T-lymphocyte antigen-4 (CTLA-4, ipilimumab), programmed death protein 1 (PD-1, pembrolizumab, nivolumab), and programmed death ligand-1 (PD-L1, atezolizumab, avelumab, durvalumab).
These medications upregulate the immune system and cause autoimmune-like side effects. Ophthalmic side effects most frequently manifest as uveitis (۱%) and dry eye (۱–۲۴%). Other side effects include myasthenia gravis (n = 19 reports), inflammatory orbitopathy (n = 11), keratitis (n = 3), cranial nerve palsy (n = 3), optic neuropathy (n = 2), serous retinal detachment (n = 2), extraocular muscle myopathy (n = 1), atypical chorioretinal lesions (n = 1), immune retinopathy (n = 1), and neuroretinitis (n = 1).
Most inflammatory side effects are managed with topical or periocular corticosteroids, but advanced cases require systemic corticosteroids and cessation of checkpoint inhibitor therapy.
Conclusion: Checkpoint inhibitors enhance the immune system by releasing inhibition on T cells, with risk of autoimmune-like side effects. Ophthalmologists should include immune-related adverse events in their differential when examining cancer patients with new ocular symptoms. RETINA 0:1–۱۶, ۲۰۱۸
Progressive Retinal Detachment In Infants With Retinopathy Of Prematurity Treated With Intravitreal Bevacizumab Or Ranibizumab
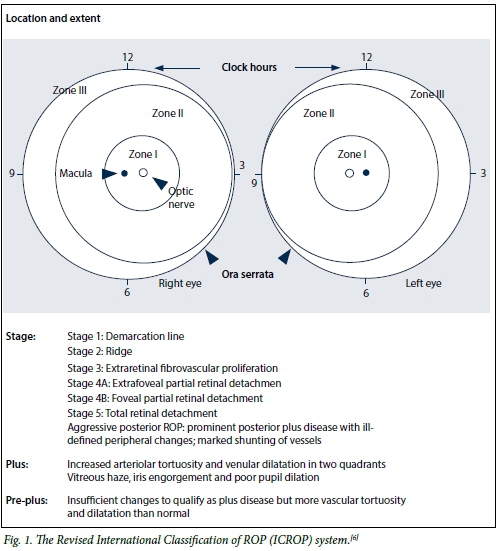
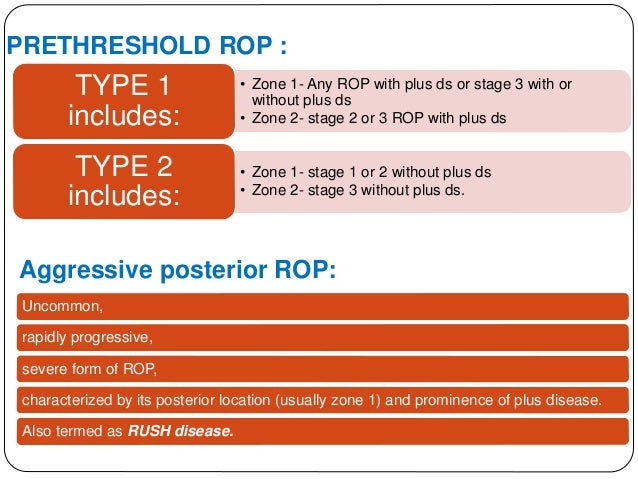
Purpose: Fibrovascular contraction and tractional retinal detachment (TRD) are recognized complications associated with the use of anti–vascular endothelial growth factor agents in vasoproliferative vitreoretinopathies. The authors characterize TRDs that developed after intravitreal bevacizumab or ranibizumab therapy for vascularly active retinopathy of prematurity.
Methods: This is an international, multicenter, interventional, retrospective, case series.
Thirty-five eyes from 23 infants were included. Inclusion required anti–vascular endothelial growth factor treatment of Type 1 retinopathy of prematurity with progression to TRD.
Results: Mean gestational age was 26 ± ۲ weeks, and mean birth weight was 873 ± ۳۴۱ g.
Mean postmenstrual age on the day of injection was 35 ± ۲ weeks. Retinal detachment was noted a mean of 70 days (median, 34; range, 4–۳۳۵) after injection. Eleven percent detached within 1 week, 23% within 2 weeks, and 49% within 4 weeks. The highest stage of retinopathy of prematurity noted was 4A in 29%, 4B in 37%, and 5 in 34% of eyes. Time to RD negatively correlated with postmenstrual age at the time of injection (Rho = 20.54; P , 0.01). Three TRD configurations were observed: 1) conventional peripheral elevated ridge or volcano-shaped Stage 5 detachment, 2) midperipheral detachment with tight circumferential vectors, and 3) very posterior detachment with prepapillary contraction. Full or partial reattachment was achieved with surgical intervention in 86% of eyes.
Conclusion: Progressive atypical TRD may occur after anti–vascular endothelial growth factor injections for retinopathy of prematurity. The configuration of the detachment varies with the extent of primary retinal vascularization present at the time of treatment. RETINA 0:1–۵, ۲۰۱۷
Dexamethasone Intravitreal Implant For The Treatment Of Recalcitrant Macular Edema After Rhegmatogenous Retinal Detachment Repair
Purpose: To investigate the efficacy of the intravitreal dexamethasone implant as the
treatment for recalcitrant macular edema after successful rhegmatogenous retinal detachment repair.
Methods: A retrospective review of the medical records was performed on 17 consecutive patients (17 eyes) with recalcitrant macular edema associated with rhegmatogenous retinal detachment repair who were treated with a single or multiple injections of an intravitreal dexamethasone 0.7-mg implant (Ozurdex; Allergan Inc) at two centers.
Main outcomes of the study were change in logarithm of the minimum angle of resolution visual acuity, measurement of central foveal thickness, and macular cube volume as measured by spectral domain optical coherence tomography and frequency of complications. Results: The mean age was 67 years (range, 51–۷۸ years). All 17 patients received previous topical therapy and ۱۲ of them had previous administration of intravitreal triamcinolone with persistence of macular edema. Baseline mean best-corrected visual acuity was 20/100 (logarithm of the minimum angle of resolution 0.75; range, 0.18–۱.۳ ±۰.۳۷) in the affected eyes. There was a statistically significant improvement in best-corrected visual acuity at 1 month (P , 0.001) and 3 months (P = 0.01). Mean baseline central foveal thickness was 505 mm, and mean macular cube volume was 10.62 mm3.
There was a statistically significant decrease in central foveal thickness and macular cube volume at 1 month (505–۲۹۰ mm, P = 0.013 and 10.62–۹.۱۳ mm3, P , 0.0001) and 3 months (P = 0.01). All patients developed recurrence of macular edema at 3 months, which required retreatment. The average number of implants was 4 (range, 1–۱۴). No adverse effects such as retinal detachment or endophthalmitis occurred. Two patients experienced an increase in intraocular pressure that was controlled with topical therapy.
Conclusion: Macular edema that occurs in eyes after successful repair of rhegmatogenous retinal detachment can be chronic and recalcitrant, and may be successfully and safely treated with the dexamethasone intravitreal implant. RETINA 0:1–۷, ۲۰۱۷
Wrinkled Vascularized Retinal Pigment Epithelium Detachment Prognosis After Intravitreal Anti-Vegf Therapy
Background/Purpose: Neovascular age-related macular degeneration (nAMD) is frequently associated with vascularized pigment epithelial detachment (v-PED). We observed a peculiar characteristic of v-PED characterized by small lacy folds of the retinal pigment epithelium, appearing as a wrinkled PED (w-PED) on spectral domain optical coherence tomography (SD-OCT). Our purpose was to describe the visual prognosis and number of intravitreal injections in w-PED compared with non-w-PED.
Methods: In this retrospective, case-control series, we reviewed retrospectively medical
records of 52 eyes of 51 patients who were consecutively included between November 1 and 30, 2015 with a previous minimum 3-year follow-up. Inclusion criteria were: neovascular age-related macular degeneration, affected with w-PED. Baseline characteristics, best-corrected visual acuity (BVCA), number of intravitreal anti-vascular endothelial growth factor injections (anti-VEGF IVT) and maximal recurrence-free interval, that is, without intravitreal anti-vascular endothelial growth factor injection, were analyzed.
A wrinkled PED (w-PED) was defined as a v-PED >200 mm in height on SD-OCT imaging, presenting with at least 4 small lacy folds on the surface of the retinal pigment epithelium.
Patients were compared with a control group, that is, patients harboring PED without wrinkle shape (non-w-PED). All patients had been treated by intravitreal anti-vascular endothelial growth factor injection of either ranibizumab (IVR) or aflibercept (IVA) using a pro re nata (PRN) protocol after three initial monthly treatments, with a minimum of follow-up of 3 years.
Results: Two groups of patients were compared, w-PED (29 eyes, from 29 patients), and non-w-PED (23eyesfrom22patients).In the w-PED group,mean BCVA evolved from 0.28 (±۰.۱۸) log MAR (20/40, range 20/25–۲۰/۶۳) at baseline, to 0.29 (±۰.۲۱) log MAR (20/40, range 20/25–۲۰/۶۳) at 1 year (P = 0.41), 0.34 (±۰.۲۶) log MAR (20/40, range 20/25–۲۰/۸۰) at 2 years (P = 0.49), 0.35 (±۰.۲۸) log MAR (20/40, range 20/25–۲۰/ ۸۰) at 3 years (P = 0.54).
In the non-w-PED group, mean BCVA was 0.40 (±۰.۲۸) log MAR (20/50, range 20/25–۲۰/۱۰۰) at baseline and decreased to 0.48 (±۰.۴۶) log MAR (20/63, range 20/20–۲۰/۱۶۰) at 1 year (P = 0.19), 0.48 (±۰.۳۵) log MAR (20/63, range 20/25–۲۰/۱۲۵) at 2 years (P = 0.02), 0.60 (±۰.۳۸) log MAR (20/80, range 20/32–۲۰/۲۰۰) at 3 years (P = 0.002).
In the w-PED group, the mean maximal documented recurrencefree interval was 7.87 (±۲.۹۴) months at Year 1, 13.5 (±۷.۵۲) at Year 2 and 14.78 (±۱۰.۷۰) at Year 3, versus 4.59 (±۲.۹۵) months at Year 1, 7.83 (±۶.۶۲) at Year 2, 8.57 (±۱۱.۱۸) at Year 3 in the non-w-PED group (P = 0.0004; 0.0101; 0.0168 respectively at Years 1, 2 and 3).
Discussion: The evolution of v-PED after intravitreal anti-vascular endothelial growth factor injection is still difficult to predict despite intense clinical research in this topic. In our study, we noticed that w-PED might be a phenotypic prognosis factor for better visual acuity and longer maximal recurrence-free interval. RETINA 0:1–۱۰, ۲۰۱۷
Optical Coherence Tomography Baseline Predictors For Initial Best-Corrected Visual Acuity Response To Intravitreal Antivascular Endothelial Growth Factor Treatment In Eyes With Diabetic Macular Edema The Chartres Study
Purpose: To identify baseline optical coherence tomography morphologic characteristics predicting the visual response to anti-vascular endothelial growth factor therapy in diabetic macular edema.
Methods: Sixty-seven patients with diabetic macular edema completed a prospective, observational study (NCT01947881-CHARTRES). All patients received monthly intravitreal injections of Lucentis for 3 months followed by PRN treatment and underwent bes tcorrected visual acuity measurements and spectral domain optical coherence tomography at Baseline, Months 1, 2, 3, and 6. Visual treatment response was characterized as good ($10 letters), moderate (5–۱۰ letters), and poor (,5 or letters loss). Spectral domain optical coherence tomography images were graded before and after treatment by a certified Reading Center.
Results: One month after loading dose, 26 patients (38.80%) were identified as good responders, 19 (28.35%) as Moderate and 22 (32.83%) as poor responders. There were no significant best-corrected visual acuity and central retinal thickness differences at baseline (P = 0.176; P = 0.573, respectively). Ellipsoid zone disruption and disorganization of retinal inner layers were good predictors for treatment response, representing a significant risk for poor visual recovery to anti-vascular endothelial growth factor therapy (odds ratio = 10.96; P , 0.001 for ellipsoid zone disruption and odds ratio = 7.05; P = 0.034 for disorganization of retinal inner layers).
Conclusion: Damage of ellipsoid zone, higher values of disorganization of retinal inner layers, and central retinal thickness decrease are good predictors of best-corrected visual acuity response to anti-vascular endothelial growth factor therapy. RETINA 0:1–۱۰, ۲۰۱۷
read more about disorganization of retinal inner layers :
Effects Of Intravitreal Ranibizumab And Bevacizumab On The Retinal Vessel Size In Diabetic Macular Edema
Purpose: The goal of this study was to assess the effects of a single injection of intravitreal ranibizumab (RAN) or bevacizumab (BEV) on the retinal vessel size in eyes with diabetic macular edema.
Materials and Methods: In total, 32 patients were enrolled in the RAN group, and 30 patients were included in BEV group. Each of these groups was also subdivided into two others groups: a study group and a control group. The study groups were composed of the injected eyes, whereas the noninjected fellow eyes served as the control groups. The patients underwent complete ophthalmic examinations, including optical coherence tomography and fundus fluorescein angiography, and the primary outcome measures included the central retinal artery equivalent, central retinal vein equivalent, and artery-to vein ratio.
Results: In the RAN study group (n = 32), the preinjection mean central retinal artery equivalent (175.42 mm) decreased to 169.01 mm after 1 week, and to 167.47 mm after 1 month (P , 0.001), whereas the baseline central retinal vein equivalent (235.29 mm) decreased initially to 219.90 mm after 1 week, and to 218.36 mm after 1 month (P , 0.001). In the BEV study group (n = 30), the preinjection central retinal artery equivalent (150.21 mm) decreased to 146.25 mm after 1 week, and to 145.89 mm after 1 month (P , 0.001); whereas the baseline central retinal vein equivalent (211.87 mm) decreased initially to 204.59 mm after 1 week and was 205.24 mm after 1 month (P , 0.001). The preinjection artery-to-vein ratio values changed significantly (P = 0.001) after 1 week and after 1 month in the RAN group, but no significant alteration in the artery-to-vein ratio was observed in the BEV group (P = 0.433). In both the RAN (n = 32) and BEV (n = 30) control groups, none of the 3 parameters changed throughout the study period, when compared with the baseline.
Conclusion: The results of this study showed that both RAN and BEV injections significantly constricted the retinal blood vessel diameters. RETINA 0:1–۷, ۲۰۱۷
Efficacy Of Intravitreal Ranibizumab Injections In The Treatment Of Vitreous Hemorrhage Related To Proliferative Diabetic Retinopathy.
PURPOSE:
To investigate the efficacy of intravitreal ranibizumab injections in proliferative diabetic retinopathy associated with vitreous hemorrhage (VH).
METHODS:
A prospective study including patients with proliferative diabetic retinopathy who presented with persistent VH. Vitreous hemorrhage was graded into mild, moderate, and severe. Patients were randomized into two groups: the ranibizumab group was treated with intravitreal injections of ranibizumab and the control group was assigned to observation alone.
Vitrectomy was performed if there was any aggravation of the VH in patients with mild, moderate, and severe VH or in the absence of improvement by 16 weeks in patients with moderate and severe VH.
RESULTS:
The ranibizumab group included 71 patients and the control group included 62 patients. There was a statistically significant difference in the vitrectomy rate in patients with mild-to-moderate VH (۵ patients [7.04%] and 12 patients [19.35%], respectively; P = 0.04). However, there was no statistically significant difference in the overall vitrectomy rate, and in the vitrectomy rate in severe VH (17 [23.94%] and 12 [16.90%] patients in the ranibizumab group vs. 22 [35.48%] and 10 [16.13%] patients in the control group, P = 0.14 and P = 0.83, respectively). Recurrence of the VH occurred in 22 patients in the ranibizumab group and 29 patients in the control group (P = 0.06). Better visual acuity measurements were recorded on all follow-up visits in the ranibizumab group (P ≤ ۰.۰۴).
CONCLUSION:
Intravitreal ranibizumab injections could be considered in proliferative diabetic retinopathy patients with mild and moderate VH.
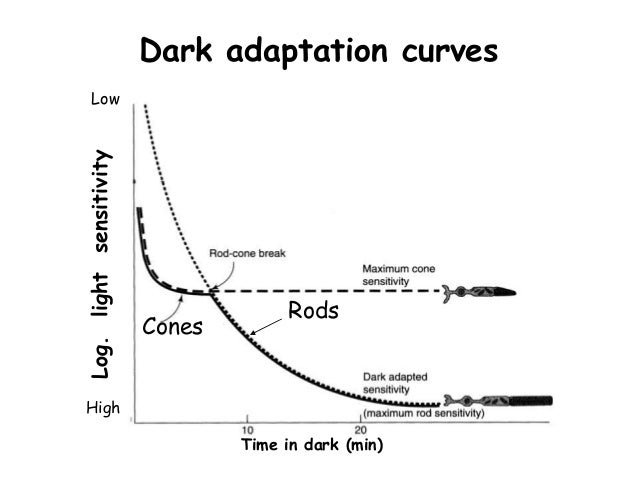
Health Conditions Linked To Age-Related Macular Degeneration Associated With Dark Adaptation
Purpose: To determine the association between dark adaption (DA) and different health conditions linked with age-related macular degeneration (AMD).
Methods: Cross-sectional study, including patients with AMD and a control group. Age related macular degeneration was graded according to the Age-Related Eye Disease Study (AREDS) classification. We obtained data on medical history, medications, and lifestyle. Dark adaption was assessed with the extended protocol (20 minutes) of AdaptDx (MacuLogix). For analyses, the right eye or the eye with more advanced AMD was selected. Multivariate linear and logistic regressions were performed, accounting for age and AMD stage.
Results: Seventy-eight subjects (75.6%AMD; 24.4% controls) were included. Multivariate assessments revealed that body mass index (BMI; b =0.30, P = 0.045), taking AREDS vitamins (b =5.51, P , 0.001), and family history of AMD (b =2.68, P = 0.039) were significantly associated with worse rod intercept times. Abnormal DA (rod intercept time $ 6.5 minutes) was significantly associated with family history of AMD (b = 1.84, P =0.006), taking AREDS supplements (b =1.67, P = 0.021) and alcohol intake (b =0.07, P = 0.017).
Conclusion: Besides age and AMD stage, a higher body mass index, higher alcohol intake, and a family history of AMD seem to impair DA. In this cohort, the use of AREDS vitamins was also statistically linked with impaired DA, most likely because of an increased severity of disease in subjects taking them. RETINA 0:1–۱۱, ۲۰۱۷
High-Dose High-Frequency Aflibercept For Recalcitrant Neovascular Age-Related Macular Degeneration
Purpose: To determine the efficacy of monthly (0.1 mL/4 mg) aflibercept for refractory neovascular age-related macular degeneration (wet age-related macular degeneration).
Methods: This was a retrospective interventional case series in which patients with wet age-related macular degeneration were treated with step wise dose escalation. Nonvitrectomized patients resistant to monthly (Q4W) ranibizumab/bevacizumab were switched to 2 mg aflibercept every 8 weeks. With resistance, they were escalated to Q4W 2 mg aflibercept, then Q4W 4 mg (high dose high frequency, 4Q4W) aflibercept.
Resistance was defined as >= 2 recurrences after being dry following >= 3 injections or persistent exudation on treatment of >= 5 injections.
Results: Thirty-three eyes of 28 patients were treated with 4Q4W aflibercept and followed for a mean of 16 months. A dry retina (no intraretinal or subretinal fluid) was achieved after initiating 4Q4W aflibercept treatment at a mean of 3.8 months. Central foveal thickness, maximum foveal thickness, intraretinal fluid, subretinal fluid, and retinal pigment detachment height decreased significantly at 1 month after initiating the 4Q4W aflibercept, and the morphologic therapeutic effect was sustained until the last visit. Forty-five percent of eyes had one or more lines of vision improvement. New geographic atrophy developed in 9% of eyes during follow-up. No ocular or systemic adverse events occurred after initiating 4Q4W aflibercept.
Conclusion: Intravitreal high-dose high-frequency aflibercept is an effective treatment for patients with refractory wet age-related macular degeneration. RETINA 38:1156–۱۱۶۵, ۲۰۱۸
Predictors Of Refractory Macular Edema After Branch Retinal Vein Occlusion Following Intravitreal Bevacizumab
Purpose: To evaluate the predictors of refractory macular edema (ME) that develops despite multiple bevacizumab injections in patients with branch retinal vein occlusion (BRVO).
Methods: A total of 107 patients who followed at least 2 years were assigned to 2 groups: a refractory group (n = 56) and a responsive group (n = 51). Baseline characteristics, treatment response at 3 months, and fluorescein angiographic findings at 6 months were compared. Then we tried to identify factors associated with refractory ME development.
Results: Compared to the responsive group, the refractory group had
- older age,
- longer pre-treatment duration, and
- shorter occlusion distance from disk.
At 3 months, the refractory group exhibited lower visual acuity, thicker central retinal thickness (CRT), and larger proportion of external limiting membrane (ELM) and outer plexiform layer disruption. After 6 months, proportion of unresolved vein occlusion, macular ischemia, number of microaneurysms, and non-perfusion areas were higher in the refractory group.
Refractory ME was associated with pre-treatment duration >=3 months, short occlusion distance from disk, thick CRT and ELM disruption at 3 months, and unresolved vein occlusion at 6 months.
Conclusion: If BRVO-ME patients exhibit the above-mentioned characteristics, they may have refractory ME, which should inform treatment decisions. RETINA 0:1–۹, ۲۰۱۷
Macular Edema After Cataract Surgery In Eyes With Preoperative Retinal Vein Occlusion.
Abstract:
Purpose:To evaluate the incidence of pseudophakic macular edema (PME) in eyes with a history of retinal vein occlusion before cataract surgery and to identify any associated risk factors.
Methods:The records of 21,332 eyes that underwent cataract surgery were retrospectively reviewed. Eyes that had retinal vein occlusion preoperatively with no evidence of macular pathology on optical coherence tomography at the time of surgery and no macular edema treatment at least 6 months before surgery were included. Eyes with diabetes or diabetic retinopathy, those with a history of previous intraocular surgery or with intraoperative complications, and those administered glaucoma and nonsteroidal antiinflammatory eye drops were excluded.
Results:Pseudophakic macular edema developed in 31 (۲۷.۴%) of 113 eyes within 3 months of cataract surgery. Mean visual acuity for eyes with PME (0.48 logarithm of the minimum angle of resolution [logMAR; 20/60 Snellen equivalent]) at 3 months after surgery was significantly worse than that for eyes without PME (0.28 logMAR; 20/38, P = 0.۰۲۰). However, there was no significant difference in the visual acuity between the 2 groups 6 months after the surgery. Taking into consideration various baseline factors, a history of previous treatment of macular edema was significantly associated with an increased risk of PME (odds ratio, 11.022; 95% confidence interval, 7.258–۱۷.۷۱۲; P = 0.۰۰۹). A higher number of intravitreal injections used to treat macular edema also significantly increased the risk of PME (odds ratio, 1.902; 95% confidence interval, 1.032–۴.۲۲۷; P = 0.۰۳۱).
Conclusion:Pseudophakic macular edema frequently developed after phacoemulsification cataract surgery in patients with a history of retinal vein occlusion. The risk of PME further increased when the patient had undergone macular edema treatment and had a higher prevalence of intravitreal injection treatment.
Polypoidal Choroidal Vasculopathy Upon Optical Coherence Tomographic Angiography
Abstract:
Purpose:To study polypoidal lesions and branching choroidal vascular networks in eyes with polypoidal choroidal vasculopathy by optical coherence tomography (OCT)–based angiography (OCTA).
Methods:In the observational cross-sectional study, patients with polypoidal choroidal vasculopathy, as diagnosed by indocyanine green angiography, underwent OCTA.
Results:Thirty-two eyes of 31 patients with an age of 61.1 ± ۷.۶ years were included. Branching choroidal vascular networks were detected by indocyanine green angiography and OCTA in 25 of 32 (۷۸ ± ۷۳%) and in 30 of 32 (۹۴ ± ۴%) eyes, respectively, with a marginally significant difference ( P = 0.۰۶) in the detection rate between both techniques. A total of 72 polyps (area, 0.06 ± ۰.۰۶ mm ۲ ; range, 0.01–۰.۲۷ mm ۲ ) were detected by indocyanine green angiography, and they were consistently present on the OCTA images.
By moving the reference level in the OCT angiograms to the corresponding layer, the polypoidal lesions showed cluster-like structures in 53 of 72 polypoidal lesions (74%).
In 60 of the 72 polypoidal lesions (۸۳%), cluster-like structures were detected in the en face structural OCT images at the reference plane of the OCTA images. On the cross-sectional OCT images, some internal channels of flow were seen in 50 of the 72 polypoidal lesions (69%). Larger size of the polypoidal lesions was associated with a higher prevalence of cluster-like structures on the OCTA images, some internal channels of flow on the en face structural images, and clustered vascular structures on the cross-sectional OCT images.
Conclusion:In conclusion, OCTA is a useful technique for the noninvasive detection of branching choroidal vascular networks including visualization of details such as cluster-like structures and flow.
In some eyes, OCTA was superior to indocyanine green angiography to detect polypoidal choroidal vasculopathy and to show branching choroidal vascular networks.
read more here :
Polypoidal Choroidal Vasculopathy Associated With Central Serous Chorioretinopathy: Pachychoroid Spectrum Of Diseases
Abstract:
Purpose:To study multimodal imaging features of polypoidal choroidal vasculopathy (PCV) associated with central serous chorioretinopathy (CSC) in the same eye.
Methods:A retrospective observational study of cases of suspected PCV which underwent indocyanine green angiography, fundus fluorescein angiography and optical coherence tomography was done, to look for simultaneous typical CSC-like active leak in the same eye. The relevant history, best-corrected visual acuity, optical coherence tomography, fundus fluorescein angiography, and indocyanine green angiography findings were analyzed.
Results:From 226 patients reviewed, 195 patients had PCV from which 6 eyes (3.07%) with features of PCV associated with typical CSC-like active leak in the same eye were identified; 3 men and 3 women with a mean age of 62.6 years. Optical coherence tomography showed notched pigment epithelial detachment in two and irregular peaked pigment epithelial detachment in four cases with subretinal fluid and/or subretinal haemorrhage over a thick choroid with dilated outer choroidal vessels. Fundus fluorescein angiography showed stippled hyperfluorescence at polyp area and a separate typical CSC-like active leak—Inkblot in three and Smokestack in three cases. On indocyanine green angiography, multiple polyps were noted with choroidal hyperpermeability in late phase at the site of CSC leak.
Conclusion:The coexistence of PCV with typical CSC-like active leaks and a thick choroid in the same eye simultaneously provides strong evidence that these diseases have an association and support the hypothesis that these conditions may originate from predisposed thick choroid.
read more about Pachychoroid Spectrum :
Dysfunctional Autonomic Regulation Of The Choroid In Central Serous Chorioretinopathy
Abstract:
Purpose:
To study the effect of changing perfusion pressures on retinal and choroidal structure in central serous chorioretinopathy (CSC).
Methods:
This prospective observational case series included seven healthy volunteers (14 eyes) and seven patients (14 eyes) with CSC. Each patient underwent spectral domain optical coherence tomography with enhanced depth imaging in the upright (sitting) and supine positions. Image segmentation focused on central macular thickness, subretinal fluid, total macular volume, choroidal thickness, and choriocapillaris thickness. Blood pressure and heart rate were measured in the upright and supine positions.
Results:
Choriocapillaris thickness was thicker in CSC participants (۳۴.۲۳ μ m; range, 30.9–۳۶.۵ μ m) compared with healthy controls (13.96 μ m; range, 7.15–۲۳.۸۷ μ m) ( P ≤ ۰.۰۰۱). The choroid was similarly thicker in CSC participants (۳۷۱.۴ μ m; range, 200.2–۴۵۹.۴ μ m) compared with healthy controls (231.4 μ m; range 161.8–۲۸۷.۵ μ m) ( P ≤ ۰.۰۰۱).
Choroidal thickness increased in patients with CSC when transitioning from upright (371.4 μ m) to supine (377.8 μ m) ( P ≤ ۰.۰۱). By contrast, there was an 11.97% decrease in choroid thickness in normal controls when transitioning from upright (231.4 μ m) to supine (203.9 μ m). There were no significant hemodynamic changes.
Conclusion:
We demonstrated that choroidal thickness increased in response to increased perfusion pressures in patients with CSC and not in normal controls. These findings likely represent an autonomic dysregulation of choroidal blood flow in patients with CSC.
Classification Of Haller Vessel Arrangements In Acute And Chronic Central Serous Chorioretinopathy Imaged With En Face Optical Coherence Tomography
Abstract:
Purpose:
To compare the prevailing patterns of Haller vessel arrangements at the posterior pole between healthy eyes and those with central serous chorioretinopathy (CSC) using en face optical coherence tomography.
Methods:
Eyes of normal subjects and patients with acute or chronic CSC underwent optical coherence tomography imaging (RTVue 100; Optovue Inc, Fremont, CA). En face sections at the level of the Haller layer were classified by two masked graders into five mutually exclusive morphologic categories (temporal herringbone, branched from below, laterally diagonal, double arcuate, and reticular). The relative prevalence of each Haller vessel arrangement pattern was determined for each phenotype.
Results:
Numbers of eyes examined were as follows: 154 eyes of 77 normal subjects; 41 eyes of 31 patients with acute CSC; and 39 eyes of 33 patients with chronic CSC. The mean age of participants was 44.4 ± ۱۴.۶ years for healthy subjects (M:F = 37:40), 48.5 ± ۸.۲ years (M:F = 24:7) for acute CSC, and 65.3 ± ۱۳.۱ years (M:F = 28:5) for chronic CSC. The relative prevalence of each Haller vessel arrangement pattern differed by phenotype. The temporal herringbone pattern was most prevalent in healthy eyes (49.2%), whereas a reticular pattern was most prevalent in eyes with acute and/or chronic CSC (combined, 48.8%).
Conclusion:
A significant difference was observed in the prevalence of respective Haller vessel arrangement patterns between eyes of normal subjects and those of patients with either acute or chronic CSC. Although further study is needed to determine the mechanistic factors underlying these differences, and the hemodynamic implications, our data suggest that en face optical coherence tomography may find a formal role in choroidal disease classification.
read even more here :
Five different patterns in healthy left eyes observed using en face OCT analysis (upper); the pattern outline is shown below (bottom).
Pattern 1 (temporal herringbone) represented 49.2% of the reference plane, pattern 2 (branched from below) and pattern 3 (laterally diagonal) represented 14.2% of the reference plane, pattern 4 (doubled arcuate) represented 11.9% of the reference plane, and pattern 5 (reticular feature) was observed in 10.5% of the reference plane.
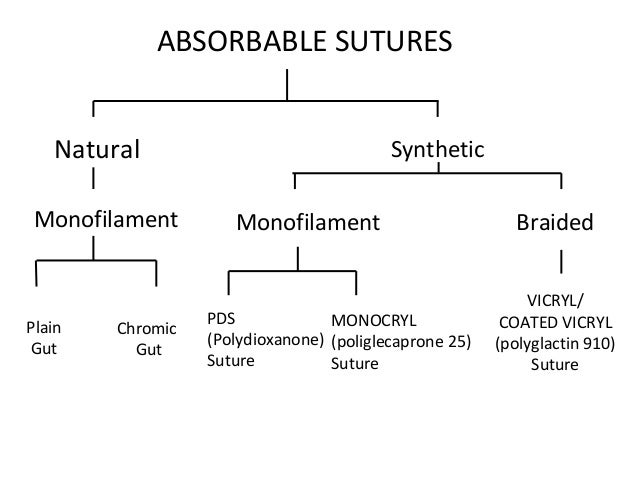
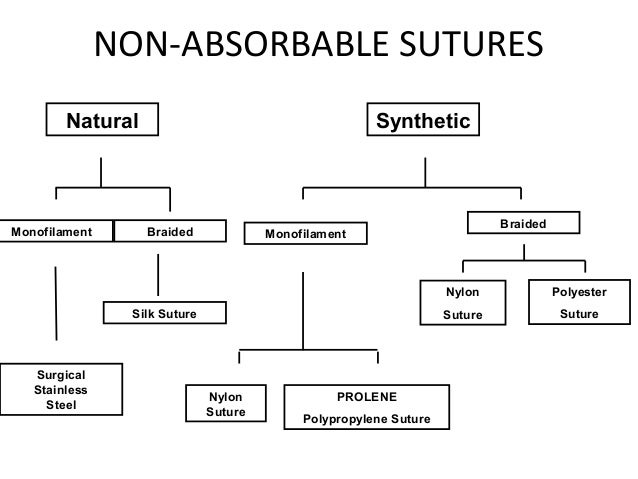
A Prospective, Randomized Trial Comparing Plain Gut To Polyglactin 910 (Vicryl) Sutures For Sclerotomy Closure After 23-Gauge Pars Plana Vitrectomy
Abstract:
Purpose:To report a prospective, randomized comparative study assessing clinical outcomes of plain gut versus polyglactin 910 (PG910) sutures for sclerotomy closure after 23-gauge pars plana vitrectomy.
Methods:A single-masked, randomized, prospective study was undertaken with 49 eyes of 49 patients undergoing 23-gauge pars plana vitrectomy randomized to sclerotomy closure with either plain gut suture, PG910 (Vicryl) suture or a combination of the two. Assessment was based on both a postoperative pain scale and a standardized assessment of scleral inflammation at each suture site.
Results:No wound leakage was noted postoperatively in any patient. Across all groups, scleral inflammation was significantly higher at the PG910 suture sites compared with the plain gut suture sites at both the 1-week ( P = 0.۰۴) and 1-month postoperative visits ( P < 0.001). Patients with PG910 sutures reported greater pain at the 1-month postoperative visit than those with plain gut sutures ( P = 0.۰۱۸).
Conclusion:This prospective study suggests improved tolerability and reduced inflammation using plain gut suture compared with an 8-0 PG910 suture to close 23-gauge sclerotomies.
learn more about sutures materials here :
Correlation Between Preoperative En Face Optical Coherence Tomography Of Photoreceptor Layer And Visual Prognosis After Macular Hole Surgery
Abstract:
Purpose:To investigate the correlation between preoperative en face spectral domain optical coherence tomography findings of the photoreceptor layer with restoration of foveal microstructure and visual acuity in repaired macular holes.
Methods:Medical records of 106 patients with surgically closed macular holes were retrospectively reviewed. Preoperative OCT slabs of the external limiting membrane (ELM) and ellipsoid zone (EZ) were generated using embedded tools. All patients were classified into two groups according to the presence of preoperative retinal pigment epithelium protrusion seen as hyperreflective spots in EZ slab. Visual acuity, homogenous reflectivity, and glial proliferation in the ELM and EZ slabs were followed for 12 months.
Results:Baseline hyperreflective spots in the EZ slab was observed in 51 (48.1%) eyes. Postoperative homogenous reflectivity and glial proliferation were related to the presence of baseline hyperreflective spots. Vision improvement was significantly greater in the absence of hyperreflective spots group from 9 months after the operation. In logistic regression analysis, the area of hyperreflective spots was significantly associated with foveal homogenous reflectivity at 12 months ( P = 0.۰۰۴).
Conclusion:Preoperative hyperreflective spots in en face EZ slab might be indicative of functional and anatomical restoration after macular hole surgery.
In our study, the eyes that had foveal glial proliferation showed worse postoperative BCVA, which is consistent with previous studies. In addition, presence of baseline hyperreflective spots group showed higher foveal glial proliferation over postoperative 12 months.