QUESTIONS
1–4
A 45-year-old male complains of slowly progressive decreased vision in his left eye for 2 months. Visual acuity is 20/200. His fundus examination and OCT are shown in Figures 12-1A and B.

FIGURE 12-1A–B
1 Which of the following best represents the pathophysiology of this patient’s condition?
A) Embolic phenomenon
B) Thrombosis at the level of the lamina cribrosa
C) Carotid stenosis
D) Compression of the central retinal vein due to an atherosclerotic arteriole
2 All of the following would be acceptable in the management of this patient except:
A) dexamethasone intravitreal implant (Ozurdex™)
B) vitrectomy with sheathotomy
C) intravitreal anti-VEGF agent
D) gonioscopy
3 Which of the following is the most serious vision-threatening complication of this condition?
A) Cataract progression
B) Retinal detachment
C) Rubeosisiridis with secondary neovascular glaucoma
D) Refractive shift
4 All of the following systemic conditions may be associated with this condition, except:
A) hypertension
B) protein C/S deficiency
C) abnormal serum electrophoresis
D) low serum homocysteine
1 B) Thrombosis at the level of the lamina cribrosa
Figure 12-1A shows the classic appearance of a CRVO with dilated and tortuous retinal vasculature coupled with four quadrants of intraretinal hemorrhages.
The pathophysiology of CRVO is due to thrombosis at the level of the lamina cribrosa. In contrast, compression of a retinal vein by a retinal arteriole is the pathophysiology of a branch retinal vein occlusion (BRVO, choice D), not CRVO.
Embolic phenomena are more likely to cause arterial occlusions such as BRAO and/or CRAO stemming from the carotid artery or heart.
Carotid stenosis may give a similar appearance to CRVO; however, it more likely may result in the ocular ischemia syndrome (OIS), in which the fundus appearance has dilated, but not tortuous retinal vasculature, and there tend to be smaller, more mid–peripheral retinal hemorrhages.
2 B) Vitrectomy with sheathotomy
The initial management of a CRVO should include gonioscopy to exclude the presence of neovascularization of the angle (NVA), which may indicate neovacular glaucoma (NVG).
Based on the GENEVA Study, the dexamethasone intravitreal implant is FDA-approved for the treatment of macular edema secondary to CRVO. Complications of intravitreal steroids include cataract progression and raised intraocular pressure. Based on the CRUISE Study, intravitreal ranibizumab is FDA-approved for the treatment of macular edema secondary to CRVO.

3 C) Rubeosisiridis with secondary neovascular glaucoma
Rubeosis and secondary neovascular glaucoma may result in irreversible optic nerve damage and severe vision loss. Therefore, prompt treatment with ocular antihypertensives and possibly filtration surgery may be required for glaucoma management. The underlying cause of the rubeosis must be treated with prompt PRP. Fortunately, in the era of anti-VEGF agents, this sight-threatening complication is less frequently encountered.
4 D) Low serum homocysteine
The majority of CRVOs are associated with hypertension. However, in the younger population, a secondary systemic etiology may be the cause such as protein C/S deficiency, or elevated (not low) serum homocysteine, or a hyperviscosity syndrome such as multiple myeloma or Waldenstrom’s.
5
A 36-year-old asymptomatic male is referred by his optometrist for the following ocular findings (Fig. 12-2). All of the following historical facts may be pertinent in determining the underlying diagnosis except:

FIGURE 12-2
A) history of liver transplantation
B) history of multiple, nonspecific episodes of weakness and numbness
C) history of high-risk sexual behavior
D) history of polydipsia, polyphagia, polyuria
Figure 12-2 shows the appearance of multiple peripapillary cotton-wool spots in an asymptomatic patient that are characteristic of interferon retinopathy. Interferon is a medication often used in patients with a history of liver transplantation (choice A).

Fundus photographs of both eyes at presentation, demonstrating multiple peripapillary cotton-wool spots bilaterally
Although the differential diagnosis of cotton-wool spots is large, the most common etiologies include diabetes (choice D), and hypertension. Other causes of this appearance would include HIV (choice C). Choice B refers to a patient with multiple sclerosis, who would not be expected to have this fundus appearance. Patients with MS may develop optic neuritis and/or intermediate uveitis.
5 B) History of multiple, nonspecific episodes of weakness and numbness
QUESTIONS
6 and 7
A 73-year-old female with a history of well-controlled diabetes recently underwent uncomplicated phacoemulsification with a posterior chamber intraocular lens and complains of blurry vision. Best-corrected visual acuity (BCVA) is 20/60. Her fluorescein angiogram and OCT are provided in Figure 12-3.

FIGURE 12-3
6 Which retinal layer accounts for the appearance of this patient’s vision loss?
A) Nerve fiber layer
B) Outer plexiform
C) Inner plexiform
D) Outer nuclear
7 All of the following are acceptable treatment options for this patient’s vision loss except:
A) topical prednisolone
B) topical NSAID
C) focal grid laser
D) observation
6 B) Outer plexiform
Figure 12-3 shows a fluorescein angiogram of classic petalloid hyperfluorescence. The “petalloid” leakage pattern on IVFA is due the accumulation of serous fluid in the outer plexiform layer of the retina, which is seen on the spectral-domain OCT image.
7 C) Focal grid laser
Approximately 1% of patients undergoing routine phacoemulsification may develop the Irvine–Gass syndrome, or postcataract CME. The natural history of untreated CME is quite good, but may take up to 6 to 9 months. Generally accepted methods of treatment include observation, topical steroids, and/or topical NSAIDs.
Focal grid laser would not be indicated in this setting, unless there was concominant diabetic macular edema with leaking microaneursyms on IVFA.
QUESTIONS
8–11
A 73-year-old Caucasian female complains of sudden, painless vision loss in her left eye. BCVA measures 20/20 in her right eye and 20/60 in her left eye. Her fundus photos and early and late fluorescein angiogram are provided in Figure 12-4A. The OCT of her left eye is provided in Figure 12-4B.

FIGURE 12-4A–B
8 All of the following are FDA-approved for the treatment of her condition except:
A) intravitreal bevaziumab (Avastin™)
B) intravitreal ranibizumab (Lucentis™)
C) intravitreal aflibercept (Eylea™)
D) intravenous verteporfin (Visudyne™)
9 According to the Comparison of Age-Related Macular Degeneration Treatments Trial (CATT), which of the following is true?
A) Intravitreal bevacizumab is superior to ranibizumab
B) Intravitreal ranibizumab is superior to bevacizumab
C) Intravitreal bevacizumab is safer than ranibizumab
D) Intravitreal bevacizumab is noninferior to ranibizumab
10 What is the approximate incidence of postintravitreal injection endophthalmitis?
A) 1 in 7,500
B) 1 in 2,500
C) 1 in 10,000
D) 1 in 5,000
11 According to the ANCHOR clinical trial regarding the use of intravitreal ranibizumab for neovascluar age-related macular degeneration (ARMD), approximately what percent of patients gain at least three lines of vision after 2 years of therapy?
A) 10%
B) 50%
C) 90%
D) 30%
8 A) Intravitreal bevacizumab (Avastin™)
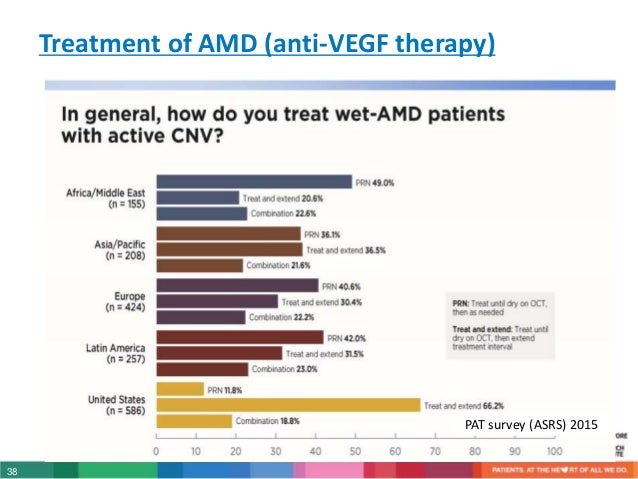
The treatment of neovascular (wet) ARMD has revolutionized with the advent of intravitreal anti-VEGF agents. As of 2013, both intravitreal ranibizumab (Lucentis™, Genentech, South San Francisco) and aflibercept (Eylea™, Regeneron, NY) are FDA-approved for the treatment of neovascular ARMD.
Visudyne™ (photodynamic therapy, PDT) is an older treatment modality that is FDA-approved for the treatment of wet ARMD, but was shown to have inferior visual outcomes compared to intravitreal ranibizumab in the ANCHOR study.
According the PAT survey in 2012, approximately 67% of retina specialists in the United States use intraviteral bevacizumab off-label as first-line treatment of wet ARMD.
9 D) Intravitreal bevacizumab is noninferior to ranibizumab.
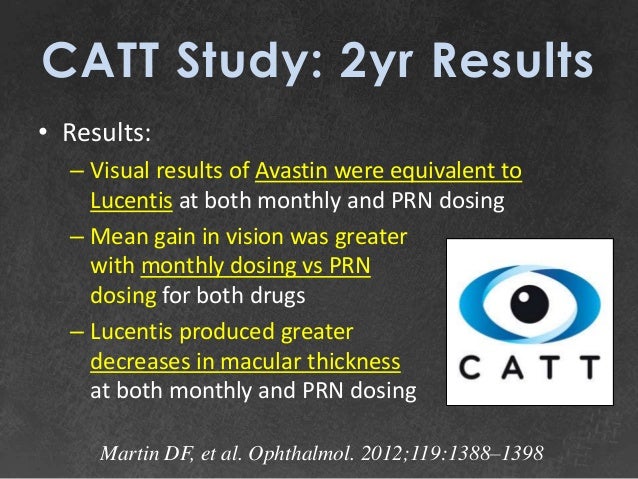
The CATT was a large, prospective, multicenter, randomized, noninferiority clinical trial comparing intravitreal bevacizumab and ranibizumab for the treatment of neovascular ARMD. At the end of 2 years of treatment, bevacizumab was shown to be noninferior to ranibizumab.
The study was not designed to determine any differences in the safety between the two medicines.

10 B) 1 in 2,500
The reported incidence of endophthalmitis following intravitreal injection of anti-VEGF agents is between 1 in 2,000 and 1 in 3,000.
11 D) 30%
The anti-vascular endothelial growth factor antibody for the treatment of predominately classic choroidal neovacularization in Age-related Macular Degeneration (ANCHOR) Trial was a prospective, randomized clinical trial that compared intravitreal ranibizumab with verteporfin PDT for neovacular ARMD. At the end of 2 years of treatment, approximately 30% of patients treated with ranibizumab gained at least three lines of vision and 90% of patients lost less than three lines of vision.

12
A 33-year-old female complains of bilateral vision loss for 4 months. Visual acuity measures CF and 20/100. Her fundus photos are provided in Figure 12-5. All of the following may be associated with the development of this condition except:

FIGURE 12-5
A) disseminated intravascular coagulation
B) polyarteritisnodosa
C) retinitis pigmentosa (RP)
D) toxemia of pregnancy
Figure 12-5 shows the classic fundus appearance of choroidal infarcts that leave wedge-shaped hyperpigmented areas in the fundus. The wedge-shaped defects are thought to follow the lobular anatomy of the choroidal blood flow.
The differential diagnosis of choroidal infarction includes accelerated (malignant) hypertension, such as from toxemia of pregnancy. Other causes include disseminated intravascular coagulation, and inflammatory conditions such as polyarteritis nodosa.
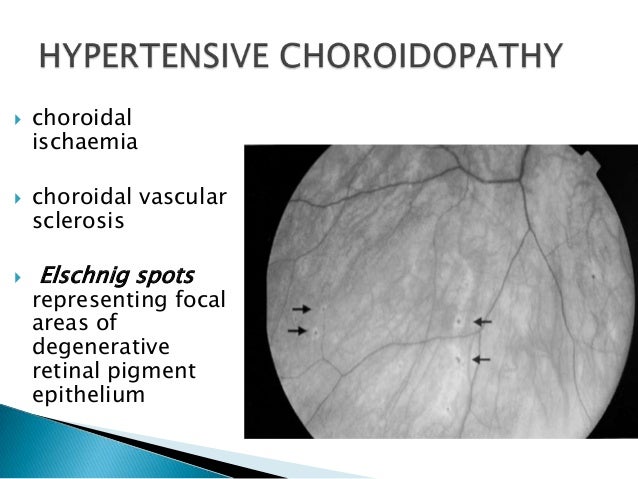

Hypertensive chorioretinopathy with Elschnig spots :
Photographs of right (a) and left (b) fundi at 3 weeks after presentation, showing bilateral optic disc oedema, subretinal exudation, right subfoveal scarring, left macular star exudate configuration, and Elschnig spots. Photographs of right (c) and left (d) fundi at 4 months after presentation and treatment, showing resolution of disc oedema, resorption of exudate, as well as residual Elschnig spots and peripapillary pigmentation. Elschnig spots in the mid-periphery, seen at 3 weeks (e) and 4 months (f) after presentation.
The appearance of RP typically causes perivascular RPE hyperpigmentation, termed “bone-spicules” with vascular attenuation, and waxy pallor of the optic nerve.
so the correct answer is C) Retinitis pigmentosa (RP) .
QUESTIONS
13–17
Match the following descriptions of the retinal layers with their corresponding labeled spectral-domain OCT layers on Figure 12-6.

FIGURE 12-6
13 This layer represents the junction between the photoreceptor inner and outer segments:
A) Z
B) X
C) V
D) W
14 A cotton-wool spot represents an infarct of this layer:
A) X
B) Y
C) V
D) Z
15 This layer is responsible for the major source of nutrition of the retinal pigment epithelium (RPE):
A) Z
B) W
C) V
D) Y
16 This layer represents interconnections between photoreceptors, bipolar, and horizontal cells:
A) W
B) Y
C) W
D) Z
17 The cell bodies in this layer have their axons in the nerve fiber layer:
A) W
B) V
C) Y
D) X
13 B) X – IS–OS junction (ellipsoid layer)
14 D) Z – nerve fiber layer
15 C) V – choriocapillaris
16 B) Y – outer plexiform layer
17 A) W – ganglion cell layer

QUESTIONS
18–20
A 34-year-old white man reports that he has had floaters for 1 week. His fundus examination is shown in Figure 12-7.

FIGURE 12-7
18 Which systemic condition is most relevant to the diagnosis?
A) Insulin-dependent diabetes mellitus since age 11
B) Uncontrolled hypertension
C) Recurrent pneumonia, weight loss, and vascular skin lesions
D) Sickle cell anemia
19 Which of the following would be seen histopathologically?
A) Retinal necrosis
B) Loss of pericytes
C) Macroaneurysms
D) Thickening and excrescences on Bruch membrane
20 What ocular complication may be associated with this condition?
A) Retinal detachment
B) Neovascular glaucoma
C) Neovascularization of the optic disc
D) Siegrist streaks
18 C) Recurrent pneumonia, weight loss, and vascular skin lesions
The fundus photo in Figure 12-7 depicts multiple cotton-wool spots and hemorrhagic necrosis of the retina after a vascular distribution. In a young patient with recurrent infections, immune deficiency should be considered, and HIV status should always be ascertained.
From 15% to 40% of patients with AIDS develop CMV retinitis. Common presenting symptoms include floaters and decreased vision. Cotton-wool spots and hemorrhages may be seen in branch retinal vein occlusions; however, there would be no associated vitritis.
19 A) Retinal necrosis
CMV retinitis is a hemorrhagic necrotizing retinitis involving all retinal layers. Intranuclear inclusion bodies may be found. Loss of pericytes and macroaneurysms can be seen with diabetes. Thickening and excrescences of Bruch membrane correspond to the drusen seen in ARMD.
20 A) Retinal detachment
CMV retinitis can lead to significant atrophy of the retina and subsequent retinal detachment. Oftentimes, multiple retinal defects are present, and the patients need long-term internal tamponade with silicone oil to prevent recurrent detachments.
Siegrist streaks are atrophic areas of the RPE overlying areas of infarction of a choroidal lobule and may be found with hypertensive retinopathy.
QUESTIONS
21 and 22
A 60-year-old woman with diabetes mellitus and hypertension reports having difficulty reading for the past 4 months. Her visual acuity is 20/25. Her fundus photograph, fluorecein angiogram, and OCT are shown in Figure 12-8.

FIGURE 12-8
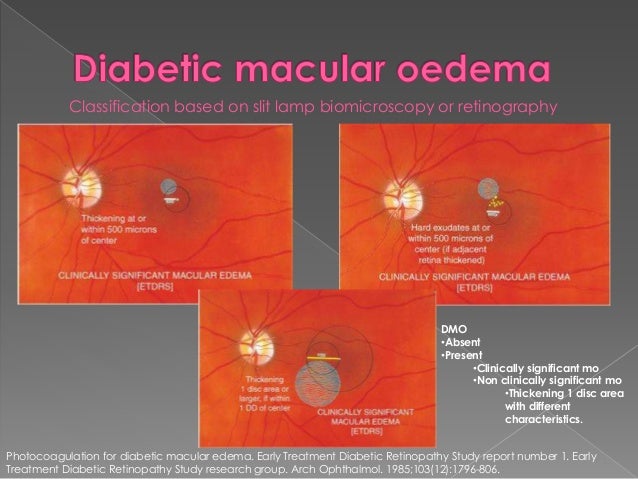
21 According to the Early Treatment of Diabetic Retinopathy Study (ETDRS), which one of the following is considered clinically significant diabetic macular edema?
A) Hard exudates within 500 µm of the fovea
B) Retinal thickening greater than 1 disk area in size and within 1 disk diameter of the center of the fovea
C) Diffuse leakage on fluorescein angiography
D) A circinate ring of exudates located 2 disk areas from the fovea
22 All of the following would be acceptable in the management of this patient except:
A) close observation with reevaluation in 2 months
B) intravitreal anti-VEGF agent
C) panretinal laser photocoagulation
D) focal laser photocoagulation
21 B) Retinal thickening greater than 1 disk area in size and within 1 disk diameter of the center of the fovea
CSME is defined as one or more of the following criteria:
1. Retinal thickening within 500 µm of the fovea.
2. Hard exudates within 500 µm of the fovea with associated retinal thickening.
3. Retinal thickening 1 disk area or greater, part of which is within 1 disk diameter of the fovea.
22 C) Panretinal laser photocoagulation
This patient has diabetic macular edema, and at the current level of visual acuity of 20/25, close observation would be an acceptable management option, giving the patient the opportunity to work on his/her glycemic control.
Recently, based on the RISE/RIDE clinical trials, intravitreal ranibizumab 0.3 mg is FDA-approved for the treatment of diabetic macular edema. In the pooled data from these identical clinical trials, approximately 40% of patients treated with ranibizumab versus 15% of patients treated with sham injection gained 15 letters after 2 years of treatment.

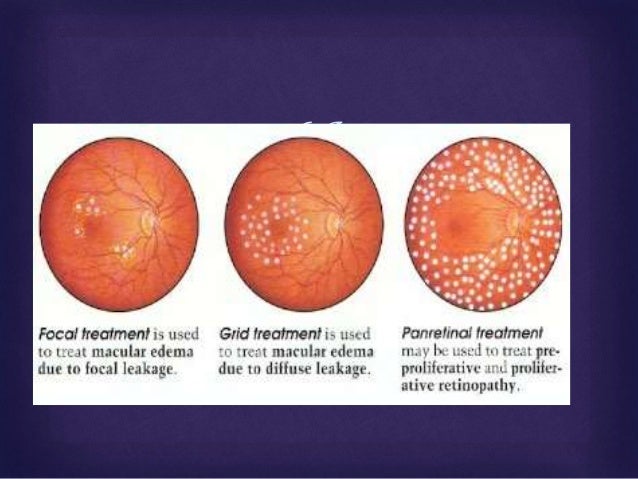
Based on the ETDRS, patients treated with focal laser photocoagulation had half the likelihood of moderate visual loss compared to untreated eyes. PRP is indicated for PDR and in fact may exacerbate macular edema.
QUESTIONS
23–25
A 7-year-old girl reports having poor vision for 2 weeks. She presents with a fundus as shown in Figure 12-9.

FIGURE 12-9
23 What historical information might be helpful in the diagnosis?
A) Prematurity with low birth weight
B) Juvenile-onset diabetes mellitus
C) Blunt trauma to orbit with a soccer ball
D) A pet cat at home
24 What laboratory studies are appropriate?
A) Urinalysis, stool for ova and parasites
B) Complete blood count (CBC), venereal disease research laboratories (VDRL) test, toxoplasma titer, viral titer screen, Bartonella IgG, and IgM
C) Antinuclear antibodies, serum protein electrophoresis (SPEP)
D) Lipoprotein, computed tomography (CT) of head and orbits
25 What treatment would you offer?
A) Triple sulfa antibiotics
B) Vitrectomy
C) Observation
D) Laser photocoagulation
23 D) A pet cat at home
The picture shown in Figure 12-9 and this history are suggestive of Leber idiopathic stellate neuroretinitis. The exact etiology of neuroretinitis is unknown but has been linked to viral infections (mumps, influenza, varicella) and other diseases (cat-scratch fever, leptospirosis).

24 B) Complete blood count (CBC), venereal disease research laboratories (VDRL) test, toxoplasma titer, viral titer screen, Bartonella IgG, and IgM
Differential diagnosis may include syphilis, toxoplasmosis of the optic nerve, diffuse unilateral subacute neuroretinitis, trauma, systemic hypertension, and diabetes mellitus.
25 C) Observation
The natural course of Leber stellate neuroretinitis is spontaneous resolution over several months. The prognosis is excellent, and over 80% of patients have visual acuity better than 20/40.
26
Which one of the following about Coats disease is true?
A) Usually bilateral
B) Associated with microphthalmia
C) Bimodal age distribution
D) Equally common between males and females
Coats disease (congenital retinal telangiectasias) tends to occur unilaterally in otherwise healthy boys. The majority of boys have the juvenile form, with a peak incidence within the end of the first decade. An adult form occurs after age 16 and may be associated with hypercholesterolemia.
Correct answer :
C) Bimodal age distribution
AAO 2018 BCSC retina :
Coats Disease Coats disease is characterized by the presence of vascular dilatations (retinal telangiectasia), including ectatic arterioles, microaneurysms, venous dilations (phlebectasias), and fusiform capillary dilatations, which are frequently associated with exudative retinal detachment. Usually only 1 eye is involved, and there is a marked male predominance (85%).
To date, researchers have not identified an associated gene or chromosome or any hereditary pattern, and no association between Coats disease and systemic disease has been found. In an eye with Coats disease, the abnormal vessels are compromised, resulting in the leakage of serum and other blood components, which accumulate in and under the retina. Any portion of the peripheral and macular capillary system may be involved. Although angiography demonstrates the presence of retinal capillary nonperfusion, posterior segment neovascularization is unusual.
The clinical findings vary widely, ranging from mild retinal vascular abnormalities and minimal exudation to extensive areas of retinal telangiectasia associated with massive leakage and exudative retinal detachment. The severity and rate of progression appear greater in children under the age of 4 years, in whom massive exudative retinal detachment with the retina apposed to the lens may simulate retinoblastoma or other causes of leukocoria (called Coats reaction; Fig 7-8; also see BCSC Section 6, Pediatric Ophthalmology and Strabismus, for the differential diagnosis of leukocoria) or xanthocoria (yellow pupil).
Patients with peripheral areas of leaky vascular anomalies typically present with lipid deposition in an otherwise angiographically normal macula, because “hard” exudate tends to accumulate in the macula. Similar findings in adults probably represent late decompensation of preexisting vascular anomalies.
Occasionally, the initial finding is a submacular lipogranuloma or subretinal fibrosis. The differential diagnosis for Coats disease may include dominant (familial) exudative vitreoretinopathy facioscapulohumeral muscular dystrophy retinopathy of prematurity (ROP) retinal hemangioblastomas (von Hippel–Lindau syndrome) For milder cases of lipid exudation, additional considerations are diabetic retinopathy, BRVO, juxtafoveal retinal telangiectasia, and radiation retinopathy.
Treatment of Coats disease generally consists of ablation with photocoagulation or cryotherapy, and, in severe cases, retinal reattachment surgery. Photocoagulation and cryotherapy are effective in obliterating the vascular anomalies and in halting progression. Several treatments may be necessary, and long-term follow-up is important to detect and treat recurrences or disease progression. Intravitreal anti–vascular endothelial growth factor (VEGF) therapy may be a useful adjunctive treatment that is resistant to ablative therapy alone.
27
Which one of the following conditions has been associated with foveal hypoplasia?
A) Choroideremia
B) Aniridia
C) Juvenile X-linked retinoschisis (JXLR)
D) Tay–Sachs disease
Foveal hypoplasia has been associated with aniridia and albinism. Choroideremia shows a generalized choroidal dystrophy. Patients with JXLR may have foveal schisis, and Tay–Sachs disease may have a cherry red spot.
B) Aniridia


QUESTIONS
28–30
A 60-year-old white woman reports having poor vision in her left eye for 4 months. Her fundus photo and OCT are shown in Figure 12-10.

FIGURE 12-10
28 What is her diagnosis?
A) Retinal detachment
B) Macular hole
C) Cystoid macular edema (CME)
D) Epiretinal membrane
29 What would fluorescein angiography show?
A) Central hypofluorescence due to blockage
B) Leakage in petalloid pattern
C) Central window defect
D) Pooling of fluorescein
30 What treatment might be offered?
A) Vitrectomy with intraocular gas injection
B) Laser photocoagulation
C) Sub-Tenon steroid injection
D) Scleral buckling procedure
28 B) Macular hole
This patient has a stage IV macular hole. The borders of the macular hole may develop a cuff of subretinal fluid. Punctate yellow deposits may exist within the defect. Idiopathic macular holes are thought to arise from tangential traction on the foveal region by the posterior cortical vitreous.

29 C) Central window defect
The RPE beneath the hole may undergo atrophy, leading to hyperfluorescence during choroidal filling on fluorescein angiography.
30 A) Vitrectomy with intraocular gas injection
Pars plana vitrectomy with internal limiting membrane (ILM) peeling and intraocular gas injection is the preferred treatment for stage IV macular holes. With surgical intervention, patients may achieve over a 90% success rate of hole closure. Often, patients are instructed to maintain postoperative prone (facedown) positioning for 3 to 7 days; however, recent literature suggests that prone positioning may not be required for successful hole closure.
31
All of the following are associated with the clinical finding shown in Figure 12-11 except:

FIGURE 12-11
A) vitreous hemorrhage (VH)
B) hypertension
C) renal cell carcinoma
D) macular edema
Figure 12-11 demonstrates a retinal arterial macroaneurysm. Macroaneurysms tend to occur in the elderly population and have been associated with systemic hypertension and atherosclerosis. Complications that may result include VH, macular edema, and exudates.
Renal cell carcinomas may be found in up to 25% of patients with von Hippel–Lindau disease. These patients present with retinal hemangioblastomas rather than with macroaneurysms. Other systemic manifestations of this phakomatosis include pheochromocytomas, pancreatic and renal cysts, and hemangioblastomas of the CNS and visceral organs.

Fundoscopic photograph illustrating a retinal hemangioblastoma (arrows).
Retinal capillary hemangioblastoma (angiomatosis retinae, previously known as retinal capillary hemangioma) is a rare autosomal dominant condition with a reported incidence of 1 in 40,000. Typically, patients are diagnosed in the second to third decades of life, although retinal lesions may be present at birth. The retinal capillary hemangioblastoma appears as a red to orange tumor arising within the retina with large-caliber, tortuous afferent and efferent retinal blood vessels .
Associated yellow-white retinal and subretinal exudates that have a predilection for foveal involvement may appear. Exudative detachments often occur in eyes with hemangioblastomas. Atypical variations include hemangiomas arising from the optic disc, which may appear as encapsulated lesions with or without pseudopapilledema, and in the retinal periphery, where vitreous traction may elevate the tumor from the surface of the retina, giving the appearance of a free-floating vitreous mass.
Fluorescein angiography of retinal capillary hemangioblastomas demonstrates a rapid arteriovenous transit, with immediate filling of the feeding arteriole, subsequent filling of the numerous fine blood vessels that constitute the tumor, and drainage by the dilated venule.
Massive leakage of dye into the tumor and vitreous can occur.
When a capillary hemangioblastoma of the retina occurs as a solitary finding, the condition is generally known as von Hippel disease. This condition is familial in about 20% of cases and bilateral in about 50%. The lesions may be multiple in 1 or both eyes.
If retinal capillary hemangiomatosis is associated with a cerebellar hemangioblastoma, the term von Hippel–Lindau syndrome is applied. The gene for von Hippel–Lindau syndrome has been isolated on chromosome 3. A number of other tumors and cysts may occur in patients with von Hippel–Lindau syndrome. The most important of these lesions are cerebellar hemangioblastomas, renal cell carcinomas, and pheochromocytomas. Genetic screening now allows for subtyping of patients with von Hippel–Lindau to determine the risk for systemic manifestations of the disease. When this diagnosis is suspected, appropriate genetic consultation and screening are critical for long-term follow-up of ocular manifestations and the associated systemic complications. Screening for systemic vascular anomalies (eg, cerebellar hemangioblastomas) and malignancies (eg, renal cell carcinoma) may reduce mortality, while aggressive screening for and early treatment of retinal hemangioblastomas may reduce late complications of exudative detachment and improve long-term visual outcomes.
The treatment of retinal capillary hemangioblastomas includes photocoagulation for smaller lesions, cryotherapy for larger and more peripheral lesions, and scleral buckling with cryotherapy or penetrating diathermy for extremely large lesions with extensive retinal detachment. External-beam and charged-particle radiotherapy have also been used. More recently, PDT has been used successfully to treat retinal capillary hemangioblastomas.
Standard verteporfin dosing coupled with both standard and modified photodynamic protocols resulted in fibrosis of the hemangiomas with secondary retinal traction and improved visual acuity in recent studies.
Recent case reports have suggested the utility of targeted antiangiogenic therapy in the management of retinal capillary hemangioblastomas. The efficacy of antiangiogenic agents in the treatment of these vascular lesions is of compelling interest to von Hippel–Lindau patients, who have a lifelong risk of developing retinal angiomas. Both systemic and intravitreal VEGF inhibitors have been used.
Reports to date suggest that the principal efficacy of VEGF inhibitors is in reducing macular edema. The impact on the actual size of the hemangiomas has been variable. Thus, the visual prognosis remains guarded for patients with large retinal lesions.
so correct answer is
31 C) Renal cell carcinoma
32
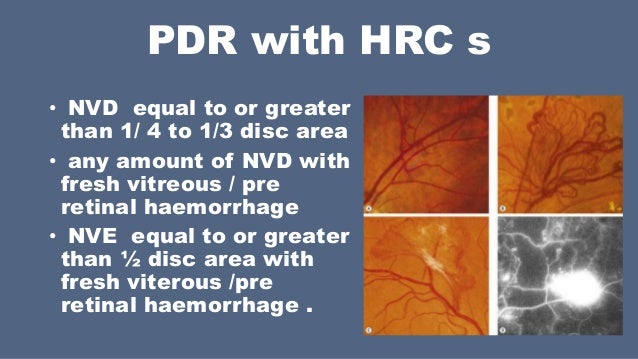
A 54-year-old poorly controlled diabetic male presents with floaters in his left eye for 1 week. BCVA measures 20/20, right eye, and 20/80, left eye. His fundus photos and angiogram are show in Figure 12-12. According to the Diabetic Retinopathy Study, all of the following meet the high-risk criteria for significant visual loss with proliferative diabetic retinopathy (PDR) except:

FIGURE 12-12
A) 1 disk area (DA) isolated neovascularization elsewhere (NVE)
B) 1/3 DA neovascularization of the disk (NVD)
C) 1/4 DA NVD with VH
D) 1/2 DA NVE with preretinal hemorrhage
Presence of three or more of the following characteristics indicates high risk for PDR as outlined by the Diabetic Retinopathy Study:
1. Any NV
2. NV on or within 1 DD of the optic disk
3. NVD greater than 1/3 disk area
4. NVE greater than 1/2 disk area
5. Vitreous or preretinal hemorrhage
So the answer is : A) 1 disk area (DA) isolated neovascularization elsewhere (NVE)
33
Which one of the following may be associated with the fundus photo and angiogram shown in Figure 12-13?

FIGURE 12-13
A) Neovascularization of the disk
B) Macular edema
C) Cotton-wool spots
D) Pigment epithelial detachment
Idiopathic juxtafoveal telangiectasis may present in two forms. A congenital form may be a subtype of Coats disease. Acquired forms may be found in middle-aged patients. The telangiectasias may be unilateral or bilateral. They are often located temporal to the fovea. Complications that may develop include macular edema, exudates, and CNV.
| Types of IJFT* | Epidemiology | Signs and symptoms | Treatment | Prognosis |
| IJFT type I | Predominantly male. Mean age 40yo. | Unilateral prominent visible telangiectatic retinal capillaries with macular edema and lipid deposition/exudate. | Laser photocoagulation may reduce exudation and stabilize vision. | Variable, majority progress to 20/70 or worse if untreated |
| IJFT type II | Equal gender predilection. Mean age 55yo. | Bilateral parafoveal graying of the retina, superficial crystalline deposits, subfoveal cystoid cavities, parafoveal telangiectasias (more evident on FA), right-angle vessels, hyperplasia of the RPE. SRNV develops in approximately 1/3 of patients. | No known treatment for non-proliferative IJFT type II.
Intravitreal anti-VEGF for SRNV. |
Variable, 2/3 of eyes will progress to 20/70 or worse associated with RPE hyperplasia or SRNV. |
| IJFT type III | Very rare | Bilateral perifoveal capillary obliteration, capillary telangiectasia, and minimal exudation, associated with systemic or cerebral disease. | Unknown due to its rarity | Variable, mostly unknown due to its rarity |
So the Answer is :
B) Macular edema
QUESTIONS
34 and 35
A 34-year-old lawyer presents with 2 days of painless blurring of vision in his right eye and the fundus shown in Figure 12-14. He had a similar episode 2 years ago.

FIGURE 12-14
34 What would the fluorescein angiogram most likely demonstrate?
A) Diffuse choroidal oozing
B) Focal leaking hot spot
C) Lacy subfoveal choroidal neovascular membrane (CNVM)
D) Leakage off optic nerve
35 Which therapy is most appropriate for this condition?
A) Observation
B) Panretinal photocoagulation (PRP)
C) Posterior sub-Tenon injection of corticosteroids
D) Scleral buckle and posterior drainage of fluid
34 B) Focal leaking hot spot
Figure 12-40 shows a case of idiopathic central serous choroidopathy (ICSC), demonstrating the classic serous elevation of the neurosensory retina over the fovea. Notice the multiple hypopigmented patches of RPE indicative of previous episodes.
Fluorescein angiography of ICSC characteristically shows a focal site of leakage from the choroid into the subsensory retinal space. The “smokestack” of dye collecting under the retina (Fig. 12-40) is the classic description (actually seen in <20% of cases).

FIGURE 12-40
Other possible causes of serous elevation of the retina include optic pits (serous detachment would be adjacent to the optic nerve), CNVMs (gray–green subretinal lesions, lipid, and hemorrhage), and serous detachments over nevi or melanoma (choroidal nevus/tumor would be visible on ophthalmoscopy).
35 A) Observation
For many cases of ICSC, the serous detachment will spontaneously resolve over 3 to 4 months. Laser photocoagulation hastens reabsorption; however, there is no difference in ultimate visual acuity compared with observation. Elevation of the retina causes a hyperopic shift, and a new refraction may temporarily help until the fluid resorbs. Periocular steroids are not beneficial. Panretinal laser photocoagulation or scleral buckling is not indicated.
36
According to the Endophthalmitis Vitrectomy Study:
A) All patients with acute endophthalmitis benefit from immediate vitrectomy.
B) Systemic antibiotics are of benefit in the final visual outcome and should be instituted in addition to intravitreal antibiotics.
C) Vitreous biopsy and injection of intravitreal antibiotics in patients with better than hand-motions vision did equally well as patients with immediate vitrectomy and injection of intravitreal antibiotics in final visual outcome.
D) In patients with light-perception only vision, neither vitrectomy nor vitreous tap was of significant benefit in final visual outcome.
C) Vitreous biopsy and injection of intravitreal antibiotics in patients with better than hand-motions vision did equally well as patients with immediate vitrectomy and injection of intravitreal antibiotics in final visual outcome.
The Endophthalmitis Vitrectomy Study specifically investigated the treatment of patients with endophthalmitis occurring within 6 weeks of cataract surgery. Patients were randomized to receive or not receive IV antibiotics and to undergo a vitrectomy/injection of intravitreal antibiotics or vitreous tap/injection of intravitreal antibiotics. The results of the study indicated the following:
1. There was no difference in final visual acuity/media clarity whether or not patients received systemic antibiotics.
2. Hand motions or better visual acuity on presentation did equally well with immediate vitreous biopsy or vitrectomy.
3. Eyes with light perception–only vision had much better visual outcome with immediate vitrectomy rather than vitreous biopsy.
QUESTIONS
37 and 38
A 25-year-old woman presents with sudden, painless vision loss in her right eye. Her visual acuity measures HM with a relative afferent pupil defect. Her fundus photos, angiogram, and OCT are shown in Figure 12-15.

FIGURE 12-15
37 Which one of the following is the least likely etiology of her condition?
A) Cardiac emboli
B) Oral contraceptives
C) Migraine
D) Atherosclerosis
38 What ocular complication may result after this condition?
A) Corneal edema
B) Staphyloma
C) Rubeosis iridis
D) CNVM
37 D) Atherosclerosis
The causes of CRAO in children and young adults differ from those of the older population. In one study, one-third of the patients had a history of migraine. Other factors include trauma (especially in males), hypercoagulable states (oral contraceptives, pregnancy), cardiac emboli, collagen vascular disorders, and IV drug abuse. In the elderly population, atherosclerotic disease is much more common.
38 C) Rubeosis iridis
The incidence of rubeosis may be as high as 15% to 20% after CRAO. These patients may also develop neovascularization of the disk and retina.
39
All findings are associated with sickle cell disease except:
A) Dalen–Fuchs nodules
B) sunbursts
C) sea fan neovascularization
D) salmon patch hemorrhages
A) Dalen–Fuchs nodules
Sickle cell retinopathy may have the following retinal findings: sunbursts (black chorioretinal scars from RPE hypertrophy and hyperplasia), salmon patch hemorrhages (subretinal blood), peripheral sea fan neovascularization, VH, and tractional retinal detachment. Angioid streaks may be associated with sickle cell disease.
Dalen–Fuchs nodules are excrescences found at the level of Bruch membrane seen in sympathetic ophthalmia
40
Degeneration of which retinal cell is the principal cause of RP?
A) Retinal pigment epithelium (RPE)
B) Rods
C) Ganglion cells
D) Cones
RP represents a collection of retinal degenerations with rod degeneration as the hallmark finding. A cone degeneration may occur secondarily.
41 All of the following are true regarding sympathetic ophthalmia except:
A) It may occur 2 years following penetrating eye injury.
B) The granulomatous uveitis occurs bilaterally.
C) Histopathologically, it is a panuveitis with sparing of the choriocapillaris.
D) The only effective treatment is enucleation of the traumatized eye.
42 All of the following may develop a similar complication leading to central visual loss except:
A) presumed ocular histoplasmosis syndrome (POHS)
B) angioid streaks
C) pathologic myopia
D) nanophthalmos
43 A 62-year-old female presents with gradually progressive distortion in her right eye. Visual acuity measures 20/70. Which lesion might lead to development of the condition shown in Figure 12-16?

FIGURE 12-16
A) Cobblestone degeneration
B) Retinal break
C) Choroidal nevus
D) Bone spicule pigmentation
44 What percentage of the population will have a cilioretinal artery?
A) 85%
B) 65%
C) 45%
D) 25%
45 The CME in which one of the following conditions would have leakage on fluorescein angiography?
A) Goldmann–Favre
B) JXLR
C) Nicotinic acid maculopathy
D) Epiretinal membrane
46 All of the following may present with subretinal, intraretinal, and preretinal hemorrhage except:
A) choroidal neovascularization (CNV)
B) sickle cell retinopathy
C) trauma
D) macroaneurysm
QUESTIONS 47–50 A 48-year-old African American man comes in for a routine eye examination, and the fluorescein angiogram pictured in Figure 12-17 is obtained.

FIGURE 12-17
47 Each of the following historical features would be helpful in confirming the etiology except:
A) hyperextensible joints
B) fractures of both femurs
C) recent splenectomy
D) headaches and nausea
48 On further examination, this patient has areas of yellowish papular skin lesions and redundant and inelastic folds of skin on the neck and thighs. What ocular manifestation of this disease might be present?
A) Optic nerve drusen
B) Arterial macroaneurysms
C) Salmon patches
D) Blue sclera
49 Which systemic complication of this condition is possible?
A) Peripheral neuropathy
B) Gastrointestinal bleeding
C) Carotid emboli and stroke
D) Weight loss and anorexia
50 Which ocular complication may occur?
A) CNV
B) RPE degeneration
C) Retinal detachment
D) VH
51 All of the following regarding choroidal melanoma are true except:
A) The presence of lipofuscin and subretinal fluid associated with the pigmented lesion may help differentiate it from a choroidal nevus.
B) A/B-scan ultrasonography of the lesion shows low internal reflectivity.
C) The liver is the most common site of metastasis.
D) Enucleation of the affected eye decreases the mortality rate.
52 Which mucopolysaccharidosis does not cause RPE degeneration?
A) Hunter’s
B) Hurler’s
C) Maroteaux–Lamy
D) Scheie’s
53 Retinal crystals may be seen with use of all of the following medications except:
A) tamoxifen
B) canthaxanthine
C) methoxyflurane
D) chloroquine
54 Findings in Stargardt disease may include all of the following except:
A) RPE atrophy in the macula
B) nonperfusion on fluoresceinangiogram
C) yellow flecks in the macula
D) yellow flecks in the peripheral retina
55 What is the most effective method to repair retinal detachments due to cytomegalovirus (CMV)?
A) Cryopexy and an intraocular gas bubble
B) Vitrectomy and endolaser
C) Scleral buckle with drainage of subretinal fluid
D) Vitrectomy and silicone oil tamponade
56 Exudative detachments occur in all of the following conditions except:
A) Vogt–Koyanagi–Harada (VKH) syndrome
B) myopia
C) toxemia of pregnancy
D) CMV retinitis
57 A copper intraocular foreign body can cause all of the following except:
A) sunflower cataract
B) Kayser–Fleischer rings
C) suppurative endophthalmitis
D) irreversibly flat ERG
58 A 67-year-old hypertensive white man awoke with acute, painless loss of vision. Examination reveals visual acuity of hand motions and an afferent pupillary defect. The fundus is shown in Figure 12-18. Which one of the following has not been advocated as a possible treatment for this condition?

FIGURE 12-18
A) Hyperbaric oxygen
B) Anterior chamber tap
C) Acetazolamide and topical β-blockers
D) Anticoagulation with Coumadin
59 Which statement regarding uveal effusion syndrome is true?
A) It occurs in eyes with abnormally short axial length.
B) It is effectively prevented by using a Flieringa ring.
C) It is treated by vitrectomy to drain choroidals.
D) Risk factors include hypertension and atherosclerosis.
60 What is the treatment for traumatic macular holes?
A) Systemic corticosteroids
B) Observation
C) Scleral buckle and vitrectomy
D) Vitrectomy and gas–fluid exchange
61 Which one of the following intraocular foreign bodies would be tolerated best?
A) Sand
B) Wood
C) Brass
D) Iron
62 Commotio retinae represents:
A) retinal edema from contusion injury
B) traumatic disruption of choroidal circulation resulting in retinal edema
C) disruption of photoreceptor elements and damage to photoreceptor cells
D) retinal edema from damage to retinal vasculature
63 What is, in order of frequency, the likelihood of traumatic retinal tears after blunt ocular injury?
1. Tears around lattice
2. Giant retinal tears
3. Inferotemporal dialysis
4. Superonasal dialysis
5. Flap tears
A) 3 > 2 > 4 > 5 > 1
B) 4 > 3 > 2 > 1 > 5
C) 3 > 4 > 2 > 5 > 1
D) 4 > 2 > 3 > 5 > 1
64 All of the following about retinopathy in shaken baby syndrome are true except:
A) Intraretinal and preretinal hemorrhages are present.
B) Has a good visual prognosis with complete healing of retinal injuries
C) May also have VH
D) Similar to central retinal vein occlusion (CRVO), Purtscher retinopathy, and Valsalva retinopathy
65 Terson syndrome may have:
A) retinal hemorrhages in patients with spontaneous or traumatic subarachnoid hemorrhages
B) VH in patients with spontaneous or traumatic subarachnoid hemorrhages
C) both A and B
D) neither A nor B
66 All of the following may be the underlying cause of the fundus appearance in Figure 12-19 except?

FIGURE 12-19
A) Severe chest compression trauma
B) Acute pancreatitis
C) Fat embolism syndrome
D) Disseminated intravascular coagulation
67 All of the following are true of the condition pictured in Figures 12-20A and B except:

FIGURE 12-20A–B
A) usually unilateral
B) increased risk of rhegmatogenous retinal detachment
C) male preponderance
D) may require treatment with laser photocoagulation
68 Persistent fetal vasculature (PFV):
A) is initially associated with a clear lens or minimal opacity that may later become densely cataractous
B) is often bilateral
C) is associated with low birth weight
D) is associated with buphthalmos
QUESTIONS 69 and 70 A 27-year-old had a ruptured right globe with uveal prolapse repaired 6 weeks before presenting with photophobia, blurry vision, and pain in the left eye.
69 Which one of the following statements regarding this patient is true?
A) Granulomatous keratic precipitates are found in both eyes.
B) Enucleation of the right eye will be beneficial in this condition.
C) This is endogenous endophthalmitis and will benefit from IV antibiotics.
D) This condition occurs in 5% of cases of penetrating ocular trauma.
70 What treatment is indicated?
A) Posterior vitrectomy of left eye
B) Oral nonsteroidal anti-inflammatory medications
C) Topical and systemic corticosteroids
D) Intravitreal injection of antibiotics
71 A 61-year-old male complains of generalized fatigue, weight loss, and fevers for several months. He has no vision complaints and visual acuity measures 20/20 OU. His fundus photo is provided in Figure 12-21. All of the following may be the cause of his underlying condition, except:

FIGURE 12-21
A) subacute bacterial endocarditis
B) leukemia
C) measles
D) collagen vascular disease
72 All of the following are associated with punctate inner choroidopathy (PIC) except:
A) myopia
B) female gender
C) viral prodrome
D) CNVMs
73 Acute posterior multifocal placoid pigment epitheliopathy (APMPPE) is associated with:
A) female preponderance
B) severe irreversible vision loss
C) viral prodrome
D) onset in fifth and sixth decades
74 Typical fluorescein angiographic findings of APMPPE are:
A) early hyperfluorescence of lesions
B) late hyperfluorescence of lesions
C) late hypofluorescence of lesions
D) leakage from optic nerve
75 Fluorescein angiographic findings of (MEWDS) include all of the following except:
A) early hypofluorescence of white dots
B) late staining of white dots
C) late disk staining
D) early hyperfluorescence of white dots
76 The most common complication of multifocal choroiditis is:
A) retinal detachment
B) CME
C) CNV
D) epiretinal membrane
77 The electrooculogram (EOG) is valuable in the detection and confirmation of the diagnosis of all of the following except:
A) carriers of Best disease
B) Best disease in the previtelliform stage
C) adult onset foveomacular vitelliform dystrophy
D) Best disease in the vitelliform stage
78 Which of the following is true regarding indocyanine green (ICG) angiography?
A) Less effective than fluorescein angiography for imaging through hemorrhage
B) More absorption of fluorescence by xanthophyll and melanin than with fluorescein
C) More effective than fluorescein angiography for imaging choroidal circulation
D) Less protein-binding than fluorescein
QUESTIONS 79–81 Match the following retinoschisis entities with the level of schisis.
79 JXLR:
A) nerve fiber layer
B) inner plexiform layer
C) outer plexiform layer
D) outer nuclear layer
80 Reticular retinoschisis:
A) nerve fiber layer
B) inner plexiform layer
C) outer plexiform layer
D) outer nuclear layer
81 Involutional or senile retinoschisis:
A) nerve fiber layer
B) inner plexiform layer
C) outer plexiform layer
D) outer nuclear layer
82 “Bull’s eye” maculopathy can occur with all of the following except:
A) cone dystrophy
B) thioridazine-induced retinopathy
C) ceroid lipofuscinosis
D) chloroquine-induced retinopathy
83 JXLR is least likely to be associated with:
A) diminished b wave with preserved a wave on ERG
B) VH
C) CME
D) peripheral retinoschisis
84 Oguchi disease is characterized by:
A) Mizuo–Nakamura phenomenon
B) autosomal recessive inheritance
C) golden brown fundus in the dark-adapted state and normal fundus in the light-adapted state
D) progressive night blindness
85 Gyrate atrophy is characterized by all of the following except:
A) ornithine transcarbamylase deficiency
B) peripheral RPE affected initially
C) high serum ornithine levels
D) abnormalities of chromosome 10
86 Which one of the following statements is false?
A) ERG amplitudes are reduced in carriers of juvenile X-linked RP.
B) ERG amplitudes are reduced in the carriers of choroideremia.
C) EOG light-peak-to-dark-trough ratio is normal in adult-onset foveomacular vitelliform dystrophy.
D) EOG light-peak-to-dark-trough ratio is reduced in carriers of Best disease.
87 All of the following may be associated with RP except:
A) autosomal dominant inheritance
B) autosomal recessive inheritance
C) optic disc hyperemia
D) posterior subcapsular (PSC) cataract
88 All of the following statements regarding albinism are true except:
A) Oculocutaneous albinism usually has autosomal dominant inheritance.
B) Ocular albinism is inherited X-linked or autosomal recessively.
C) Retinal manifestations of albinism include foveal hypoplasia and peripheral mosaic pattern of pigmentation.
D) Decussation at optic chiasm is abnormal.
89 Hermansky–Pudlak syndrome is characterized by all of the following except:
A) platelet dysfunction
B) reticuloendothelial dysfunction
C) albinism
D) Puerto Rican heritage
90 Chediak–Higashi syndrome is characterized by all of the following except:
A) platelet dysfunction
B) white forelock and silvery hair
C) albinism
D) recurrent pyogenic infections
91 What is the incidence of retinal tear in an eye with posterior vitreous detachment and VH?
A) 90%
B) 67%
C) 50%
D) 25%
92 Which one of the following poses the highest risk for retinal detachment?
A) Myopia
B) Retinal detachment in the fellow eye
C) Lattice degeneration
D) Family history of retinal detachment
93 What is the incidence of retinal detachment in fellow eyes of patients with giant retinal tears?
A) 50%
B) 25%
C) 100%
D) <5%
94 All of the following regarding toxoplasma retinitis are true except:
A) The causative organism is a bacterium.
B) A common finding is an area of focal retinitis adjacent to a pigmented choroiretinal scar.
C) Often presents with anterior chamber as well as vitreous inflammation.
D) May be associated with CNS findings.
95 What is the most important factor for determining visual outcome in retinal detachment?
A) Presence of VH
B) Duration of detachment
C) Number of retinal breaks
D) Attachment of the macula
96 What is the most common cause of recurrent retinal detachment or failure of scleral buckling procedure?
A) Scleral buckle too large causing retinal folds and fish-mouthed tears
B) Scleral buckle too small resulting in inadequate support of tears
C) No circumferential band to support vitreous base
D) Proliferative vitreoretinopathy
QUESTIONS 97–100 Where is the most likely location for the primary retinal break in each of the following retinal detachments?
A. 12 o’clock
B. 9 o’clock
C. 3 o’clock
D. 6 o’clock
97 Figure 12-22

FIGURE 12-22
98 Figure 12-23

FIGURE 12-23
99 Figure 12-24

FIGURE 12-24
100 Figure 12-25

FIGURE 12-25
101 Which one of the following regarding exudative retinal detachments is false?
A) May occur with choroidal hemangiomas
B) May occur with choroidal melanomas
C) Should be treated with scleral buckle and vitrectomy with internal drainage of the subretinal fluid
D) Are characterized by shifting subretinal fluid
102 Tractional retinal detachments occur in all of the following except:
A) diabetes mellitus
B) familial exudative vitreoretinopathy
C) retinopathy of prematurity
D) JXLR
103 Which one of the following regarding asteroid hyalosis is false?
A) Represents precipitation of calcium soaps
B) Unilateral phenomenon predominantly
C) Patients asymptomatic
D) Systemic hypercalcem
104 A patient has synchysis scintillans. Which historical feature is most probable?
A) Previous blunt trauma with hyphema
B) Dense arcus senilis
C) Carotid atherosclerosis with a history of amaurosis
D) Cushingoid appearance from long-term steroid use
105 An intraocular bubble of which one of the following gases would last the longest?
A) Air
B) Perfluoropropane (C3F8)
C) Sulfur hexafluoride (SF6)
D) Perfluoroethane (C2F6)
106 Rate of intraocular gas expansion is fastest for:
A) air
B) 100% C3F8
C) 100% SF6
D) 14% C3F8
107 The surface tension of silicone oil against the retina is:
A) greater than C3F8 against the retina
B) greater than air against retina
C) less than SF6 against retina
D) equal to water against the retina
108 The specific gravity of silicone oil is:
A) greater than balanced salt solution
B) less than water
C) less than perfluorooctane
D) equal to vitreous
QUESTIONS 109–111 A patient had sudden loss of vision to the level of light perception in the left eye. The fluorescein angiogram is shown in Figure 12-26.

FIGURE 12-26
109 What is the most appropriate next step in evaluation?
A) Carotid Doppler ultrasound
B) CT scan of chest and abdomen
C) Erythrocyte sedimentation rate (ESR)
D) MRI of head and orbits
110 Which one of the following ERG changes would be present in this eye?
A) Decreased b-wave amplitude
B) Increased implicit time
C) Absent scotopic response
D) Flat response to a flickering stimulus
111 What is the most appropriate therapy?
A) Systemic corticosteroids and temporal artery biopsy
B) Optic nerve sheath decompression
C) Carotid endarterectomy
D) Aspirin daily
QUESTIONS 112–114 (FIG. 12-27)

FIGURE 12-27A–B
112 What would this patient most likely report?
A) Painful photophobia
B) Unilateral shimmering photopsias
C) Viral illness 2 weeks before presentation
D) Recurrent fevers
113 Which one of the following is a characteristic feature of this disorder?
A) More common in women
B) Myopic patients
C) Usually recurrent causing progressive visual loss
D) Often requires corticosteroids to hasten resolution
114 What is the most consistent finding on adjunct testing?
A) Pinpoint hyperfluorescent spots that leak on fluorescein angiography
B) Enlarged blind spot on visual field testing
C) Multiple bright objects on T2 weighted MRI images
D) Profoundly reduced color vision
QUESTIONS 115–117 (FIG. 12-28) On routine examination of a 37-year-old man, you find multiple midperipheral yellowish flecks in both eyes. His fluorescein angiogram is shown in Figure 12-28.

FIGURE 12-28
115 Which one of the following is a clinical characteristic of this disorder?
A) Profoundly reduced vision in one eye
B) Profoundly reduced vision in both eyes
C) Autosomal dominant inheritance
D) Autosomal recessive inheritance
116 What is the histopathologic cause of the characteristic fluorescein appearance?
A) Choroidal nonperfusion
B) Accumulation of gangliosides in retinal ganglion cells
C) Accumulation of lipofuscin granules in the RPE
D) Diffuse thickening of Bruch membrane
117 Which one of the following electrophysiologic findings is characteristic for this condition?
A) EOG light-peak-to-dark-trough ratio is profoundly reduced.
B) Photopic ERG amplitudes are extinguished.
C) Scotopic ERG amplitudes are extinguished.
D) ERG amplitudes are often normal.
QUESTIONS 118–120 (FIG. 12-29)

FIGURE 12-29
118 What is the most likely cause of this angiographic appearance?
A) Thioridazine toxicity
B) RP
C) Cone dystrophy
D) Tay–Sachs disease
119 Toxicity from which one of the following medications may produce this angiographic appearance?
A) Chlorpromazine
B) Isoniazid
C) Chloroquine
D) Digoxin
120 What is the possible electrophysiologic finding?
A) Abnormal photopic ERG
B) Abnormal scotopic ERG
C) Supranormal a wave on scotopic ERG
D) Subnormal b wave on scotopic ERG
QUESTIONS 121–124 During which phase of the fluorescein angiogram do the following lesions initially fill? Choices may be used more than once, or not at all.
A. Choroidal
B. Early arterial
C. Arteriovenous
D. Late
121 Capillary hemangioma?
122 Malignant melanoma?
123 Neovascularization of the disk?
124 Cilioretinal artery?
125 The a, b, and c waves of the ERG originate from the following retinal structures, sequentially:
A) RPE, ganglion cells, Müller cells
B) ganglion cells, bipolar cells, RPE
C) photoreceptors, bipolar cells, RPE
D) Müller cells, ganglion cells, photoreceptors
126 The following statements about Best disease (vitelliform macular dystrophy) are correct except:
A) The EOG is pathologic in affected patients and carriers.
B) Peripheral visual fields, ERG, and dark adaptation testing are normal.
C) It is autosomal dominant.
D) It has a poor visual prognosis.
QUESTIONS 127–129 A 75-year-old lady is referred from a retinal findings in both eyes during a routine eye examination (Fig. 12-30). She denies any smoking history.

FIGURE 12-30
127 What is her risk of developing CNV in the next 5 years?
A) 12%
B) 25%
C) 50%
D) Unable to determine
128 What nutritional supplements should the patient be on?
A) Age-Related Eye Disease Study (AREDS) formulation
B) AREDS formulation without vitamin A
C) AREDS formulation with omega-3 fatty acids
D) General multivitamin
129 If she was a current or former smoker, what nutritional supplement should be avoided?
A) Vitamin C
B) Vitamin E
C) Vitamin A
D) Zinc
QUESTIONS 130 and 131 A 50-year-old diabetic woman presents with progressive blurring of vision in her right eye. A similar episode occurred in her left eye 2 months ago. She has not had previous laser photocoagulation.
130 Which of the following features are seen in the following angiogram: Figure 12-31?

FIGURE 12-31
A) Leakage from NVD and multiple NVE
B) Hypofluorescence caused by a blocking defect
C) Peripheral capillary nonperfusion
D) All of the above
131 All of the following would be acceptable in the initial management of this patient, except:
A) pars plana vitrectomy
B) PRP
C) intravitreal anti-VEGF agent
D) follow-up visit in 1 month
QUESTIONS 132–140 (Figs. 12-32–12-38)

FIGURE 12-32

FIGURE 12-33

FIGURE 12-34

FIGURE 12-35

FIGURE 12-36

FIGURE 12-37

FIGURE 12-38
132 Which one of the following is not associated with CNVMs?
A) Figure 12-32
B) Figure 12-33
C) Figure 12-34
D) Figure 12-35
133 In Figure 12-36, which investigations would be most appropriate to perform?
A) Fluorescein angiography
B) CT scan
C) Carotid Doppler and cardiac echocardiography
D) CBC and ESR
134 In which condition is laser photocoagulation inappropriate?
A) Figure 12-37
B) Figure 12-38
C) Figure 12-35
D) Figure 12-33
135 In Figure 12-34, the systemic condition most commonly associated with this disorder is:
A) diabetes mellitus
B) systemic hypertension
C) sickle cell anemia
D) thromboembolic disease
136 In reference to Figure 12-37, indications for vitrectomy could include all of the following stages of the condition except:
A) Stage I
B) Stage II
C) Stage III
D) Stage IV
137 If a posterior vitreous detachment was present in the patient seen in Figure 12-37, in what stage would this condition be?
A) Stage I
B) Stage II
C) Stage III
D) Stage IV
138 In which of the following conditions is laser treatment contraindicated?
A) Figure 12-38
B) Figure 12-36
C) Figure 12-34
D) Figure 12-33
139 In which of the following conditions may an ICG angiogram be helpful in the management of the patient?
A) Figure 12-38
B) Figure 12-36
C) Figure 12-34
D) Figure 12-33
140 All of these conditions may give rise to the fundus appearance seen in Figure 12-38 except:
A) diabetic retinopathy
B) radiation retinopathy
C) proliferative vitreoretinopathy
D) hypertensive retinopathy
141 Indications for vitrectomy in patients with diabetic retinopathy include all of the following except:
A) nonclearing VH
B) extramaculartractional retinal detachment
C) combined rhegmatogenoustractional retinal detachment
D) anterior hyaloidalfibrovascular proliferation
142 Indications for vitrectomy and membrane peeling in patients with macular epiretinal membrane include all of the following except:
A) decrease in visual acuity
B) marked retinal distortion
C) choroidal noevasclar membrane (CNVM)
D) metamorphopsia
143 Which one of the following does not have vitreous liquefication and a vitreous that appears optically empty?
A) Stickler syndrome
B) Jansen syndrome
C) Kearns–Sayre syndrome
D) Wagner syndrome
144 What is not a risk factor for the development of CNV in ARMD?
A) Age
B) Smoking
C) Male gender
D) Diet low in antioxidants and lutein
QUESTIONS 145–147 A healthy, 36-year-old white man who resides in the Eastern United States presents with a loss of central vision and metamorphopsia in his left eye, associated with a serous detachment of the macula and multiple peripheral atrophic chorioretinal scars and peripapillary chorioretinal scars (Figs. 12-39A and B). There is no inflammatory reaction in the anterior chamber or vitreous.


FIGURE 12-39A–B
145 What is the most likely diagnosis?
A) ARMD
B) Toxoplasmosis
C) POHS
D) Multifocal choroiditis and panuveitis
146 Which one of the following is not a sign of a CNVM?
A) Pigment ring or mound
B) Subretinal hemorrhage
C) Chorioretinal scar
D) Oval or round grayish-white subretinal lesion
147 In which location has laser photocoagulation not been beneficial in this condition when the CNVM is well-demarcated?
A) Extrafoveal
B) Juxtafoveal
C) Subfoveal
D) Juxtapapillary
148 Which one of the following is not a feature of lattice degeneration of the retina?
A) Liquefied vitreous overlying the lesion
B) Sclerotic vessels traversing the lesion
C) Adherence of the vitreous to the edges of the lesion
D) Operculated holes secondary to vitreous traction
149 Which phakomatosis does not have characteristic retinal findings?
A) Louis–Bar
B) Wyburn–Mason
C) Bourneville’s
D) von Hippel–Lindau
150 Macular complications of RP include all of the following except:
A) macular atrophy
B) epiretinal membrane
C) CME
D) subretinal scarring
ANSWERS
1 B) Thrombosis at the level of the lamina cribrosa
Figure 12-1A shows the classic appearance of a CRVO with dilated and tortuous retinal vasculature coupled with four quadrants of intraretinal hemorrhages. The pathophysiology of CRVO is due to thrombosis at the level of the lamina cribrosa. In contrast, compression of a retinal vein by a retinal arteriole is the pathophysiology of a branch retinal vein occlusion (BRVO, choice D), not CRVO. Embolic phenomena are more likely to cause arterial occlusions such as BRAO and/or CRAO stemming from the carotid artery or heart. Carotid stenosis may give a similar appearance to CRVO; however, it more likely may result in the ocular ischemia syndrome (OIS), in which the fundus appearance has dilated, but not tortuous retinal vasculature, and there tend to be smaller, more mid–peripheral retinal hemorrhages.
2 B) Vitrectomy with sheathotomy
The initial management of a CRVO should include gonioscopy to exclude the presence of neovascularization of the angle (NVA), which may indicate neovacular glaucoma (NVG). Based on the GENEVA Study, the dexamethasone intravitreal implant is FDA-approved for the treatment of macular edema secondary to CRVO. Complications of intravitreal steroids include cataract progression and raised intraocular pressure. Based on the CRUISE Study, intravitreal ranibizumab is FDA-approved for the treatment of macular edema secondary to CRVO.
3 C) Rubeosisiridis with secondary neovascular glaucoma
Rubeosis and secondary neovascular glaucoma may result in irreversible optic nerve damage and severe vision loss. Therefore, prompt treatment with ocular antihypertensives and possibly filtration surgery may be required for glaucoma management. The underlying cause of the rubeosis must be treated with prompt PRP. Fortunately, in the era of anti-VEGF agents, this sight-threatening complication is less frequently encountered.
4 D) Low serum homocysteine
The majority of CRVOs are associated with hypertension. However, in the younger population, a secondary systemic etiology may be the cause such as protein C/S deficiency, or elevated (not low) serum homocysteine, or a hyperviscosity syndrome such as multiple myeloma or Waldenstrom’s.
5 B) History of multiple, nonspecific episodes of weakness and numbness
Figure 12-2 shows the appearance of multiple peripapillary cotton-wool spots in an asymptomatic patient that are characteristic of interferon retinopathy. Interferon is a medication often used in patients with a history of liver transplantation (choice A). Although the differential diagnosis of cotton-wool spots is large, the most common etiologies include diabetes (choice D), and hypertension. Other causes of this appearance would include HIV (choice C). Choice B refers to a patient with multiple sclerosis, who would not be expected to have this fundus appearance. Patients with MS may develop optic neuritis and/or intermediate uveitis.
6 B) Outer plexiform
Figure 12-3 shows a fluorescein angiogram of classic petalloid hyperfluorescence. The “petalloid” leakage pattern on IVFA is due the accumulation of serous fluid in the outer plexiform layer of the retina, which is seen on the spectral-domain OCT image.
7 C) Focal grid laser
Approximately 1% of patients undergoing routine phacoemulsification may develop the Irvine–Gass syndrome, or postcataract CME. The natural history of untreated CME is quite good, but may take up to 6 to 9 months. Generally accepted methods of treatment include observation, topical steroids, and/or topical NSAIDs. Focal grid laser would not be indicated in this setting, unless there was concominant diabetic macular edema with leaking microaneursyms on IVFA.
8 A) Intravitreal bevacizumab (Avastin™)
The treatment of neovascular (wet) ARMD has revolutionized with the advent of intravitreal anti-VEGF agents. As of 2013, both intravitreal ranibizumab (Lucentis™, Genentech, South San Francisco) and aflibercept (Eylea™, Regeneron, NY) are FDA-approved for the treatment of neovascular ARMD. Visudyne™ (photodynamic therapy, PDT) is an older treatment modality that is FDA-approved for the treatment of wet ARMD, but was shown to have inferior visual outcomes compared to intravitreal ranibizumab in the ANCHOR study. According the PAT survey in 2012, approximately 67% of retina specialists in the United States use intraviteral bevacizumab off-label as first-line treatment of wet ARMD.
9 D) Intravitreal bevacizumab is noninferior to ranibizumab.
The CATT was a large, prospective, multicenter, randomized, noninferiority clinical trial comparing intravitreal bevacizumab and ranibizumab for the treatment of neovascular ARMD. At the end of 2 years of treatment, bevacizumab was shown to be noninferior to ranibizumab. The study was not designed to determine any differences in the safety between the two medicines.
10 B) 1 in 2,500
The reported incidence of endophthalmitis following intravitreal injection of anti-VEGF agents is between 1 in 2,000 and 1 in 3,000.
11 D) 30%
The anti-vascular endothelial growth factor antibody for the treatment of predominately classic choroidal neovacularization in Age-related Macular Degeneration (ANCHOR) Trial was a prospective, randomized clinical trial that compared intravitreal ranibizumab with verteporfin PDT for neovacular ARMD. At the end of 2 years of treatment, approximately 30% of patients treated with ranibizumab gained at least three lines of vision and 90% of patients lost less than three lines of vision.
12 C) Retinitis pigmentosa (RP)
Figure 12-5 shows the classic fundus appearance of choroidal infarcts that leave wedge-shaped hyperpigmented areas in the fundus. The wedge-shaped defects are thought to follow the lobular anatomy of the choroidal blood flow. The differential diagnosis of choroidal infarction includes accelerated (malignant) hypertension, such as from toxemia of pregnancy. Other causes include disseminated intravascular coagulation, and inflammatory conditions such as polyarteritisnodosa. The appearance of RP typically causes perivascular RPE hyperpigmentation, termed “bone-spicules” with vascular attenuation, and waxy pallor of the optic nerve.
13 B) X – IS–OS junction (ellipsoid layer)
14 D) Z – nerve fiber layer
15 C) V – choriocapillaris
16 B) Y – outer plexiform layer
17 A) W – ganglion cell layer
18 C) Recurrent pneumonia, weight loss, and vascular skin lesions
The fundus photo in Figure 12-7 depicts multiple cotton-wool spots and hemorrhagic necrosis of the retina after a vascular distribution. In a young patient with recurrent infections, immune deficiency should be considered, and HIV status should always be ascertained. From 15% to 40% of patients with AIDS develop CMV retinitis. Common presenting symptoms include floaters and decreased vision. Cotton-wool spots and hemorrhages may be seen in branch retinal vein occlusions; however, there would be no associated vitritis.
19 A) Retinal necrosis
CMV retinitis is a hemorrhagic necrotizing retinitis involving all retinal layers. Intranuclear inclusion bodies may be found. Loss of pericytes and macroaneurysms can be seen with diabetes. Thickening and excrescences of Bruch membrane correspond to the drusen seen in ARMD.
20 A) Retinal detachment
CMV retinitis can lead to significant atrophy of the retina and subsequent retinal detachment. Oftentimes, multiple retinal defects are present, and the patients need long-term internal tamponade with silicone oil to prevent recurrent detachments. Siegrist streaks are atrophic areas of the RPE overlying areas of infarction of a choroidal lobule and may be found with hypertensive retinopathy.
21 B) Retinal thickening greater than 1 disk area in size and within 1 disk diameter of the center of the fovea
CSME is defined as one or more of the following criteria:
1. Retinal thickening within 500 µm of the fovea.
2. Hard exudates within 500 µm of the fovea with associated retinal thickening.
3. Retinal thickening 1 disk area or greater, part of which is within 1 disk diameter of the fovea.
22 C) Panretinal laser photocoagulation
This patient has diabetic macular edema, and at the current level of visual acuity of 20/25, close observation would be an acceptable management option, giving the patient the opportunity to work on his/her glycemic control. Recently, based on the RISE/RIDE clinical trials, intravitreal ranibizumab 0.3 mg is FDA-approved for the treatment of diabetic macular edema. In the pooled data from these identical clinical trials, approximately 40% of patients treated with ranibizumab versus 15% of patients treated with sham injection gained 15 letters after 2 years of treatment. Based on the ETDRS, patients treated with focal laser photocoagulation had half the likelihood of moderate visual loss compared to untreated eyes. PRP is indicated for PDR and in fact may exacerbate macular edema.
23 D) A pet cat at home
The picture shown in Figure 12-9 and this history are suggestive of Leber idiopathic stellate neuroretinitis. The exact etiology of neuroretinitis is unknown but has been linked to viral infections (mumps, influenza, varicella) and other diseases (cat-scratch fever, leptospirosis).
24 B) Complete blood count (CBC), venereal disease research laboratories (VDRL) test, toxoplasma titer, viral titer screen, Bartonella IgG, and IgM
Differential diagnosis may include syphilis, toxoplasmosis of the optic nerve, diffuse unilateral subacute neuroretinitis, trauma, systemic hypertension, and diabetes mellitus.
25 C) Observation
The natural course of Leber stellate neuroretinitis is spontaneous resolution over several months. The prognosis is excellent, and over 80% of patients have visual acuity better than 20/40.
26 C) Bimodal age distribution
Coats disease (congenital retinal telangiectasias) tends to occur unilaterally in otherwise healthy boys. The majority of boys have the juvenile form, with a peak incidence within the end of the first decade. An adult form occurs after age 16 and may be associated with hypercholesterolemia.
27 B) Aniridia
Foveal hypoplasia has been associated with aniridia and albinism. Choroideremia shows a generalized choroidal dystrophy. Patients with JXLR may have foveal schisis, and Tay–Sachs disease may have a cherry red spot.
28 B) Macular hole
This patient has a stage IV macular hole. The borders of the macular hole may develop a cuff of subretinal fluid. Punctate yellow deposits may exist within the defect. Idiopathic macular holes are thought to arise from tangential traction on the foveal region by the posterior cortical vitreous.
29 C) Central window defect
The RPE beneath the hole may undergo atrophy, leading to hyperfluorescence during choroidal filling on fluorescein angiography.
30 A) Vitrectomy with intraocular gas injection
Pars plana vitrectomy with internal limiting membrane (ILM) peeling and intraocular gas injection is the preferred treatment for stage IV macular holes. With surgical intervention, patients may achieve over a 90% success rate of hole closure. Often, patients are instructed to maintain postoperative prone (facedown) positioning for 3 to 7 days; however, recent literature suggests that prone positioning may not be required for successful hole closure.
31 C) Renal cell carcinoma
Figure 12-11 demonstrates a retinal arterial macroaneurysm. Macroaneurysms tend to occur in the elderly population and have been associated with systemic hypertension and atherosclerosis. Complications that may result include VH, macular edema, and exudates. Renal cell carcinomas may be found in up to 25% of patients with von Hippel–Lindau disease. These patients present with retinal hemangioblastomas rather than with macroaneurysms. Other systemic manifestations of this phakomatosis include pheochromocytomas, pancreatic and renal cysts, and hemangioblastomas of the CNS and visceral organs.
32 A) 1 disk area (DA) isolated neovascularization elsewhere (NVE)
Presence of three or more of the following characteristics indicates high risk for PDR as outlined by the Diabetic Retinopathy Study:
1. Any NV
2. NV on or within 1 DD of the optic disk
3. NVD greater than 1/3 disk area
4. NVE greater than 1/2 disk area
5. Vitreous or preretinalhemorrhage
33 B) Macular edema
Idiopathic juxtafoveal telangiectasis may present in two forms. A congenital form may be a subtype of Coats disease. Acquired forms may be found in middle-aged patients. The telangiectasias may be unilateral or bilateral. They are often located temporal to the fovea. Complications that may develop include macular edema, exudates, and CNV.
34 B) Focal leaking hot spot
Figure 12-40 shows a case of idiopathic central serous choroidopathy (ICSC), demonstrating the classic serous elevation of the neurosensory retina over the fovea. Notice the multiple hypopigmented patches of RPE indicative of previous episodes.
Fluorescein angiography of ICSC characteristically shows a focal site of leakage from the choroid into the subsensory retinal space. The “smokestack” of dye collecting under the retina (Fig. 12-40) is the classic description (actually seen in <20% of cases).

FIGURE 12-40
Other possible causes of serous elevation of the retina include optic pits (serous detachment would be adjacent to the optic nerve), CNVMs (gray–green subretinal lesions, lipid, and hemorrhage), and serous detachments over nevi or melanoma (choroidal nevus/tumor would be visible on ophthalmoscopy).
35 A) Observation
For many cases of ICSC, the serous detachment will spontaneously resolve over 3 to 4 months. Laser photocoagulation hastens reabsorption; however, there is no difference in ultimate visual acuity compared with observation. Elevation of the retina causes a hyperopic shift, and a new refraction may temporarily help until the fluid resorbs. Periocular steroids are not beneficial. Panretinal laser photocoagulation or scleral buckling is not indicated.
36 C) Vitreous biopsy and injection of intravitreal antibiotics in patients with better than hand-motions vision did equally well as patients with immediate vitrectomy and injection of intravitreal antibiotics in final visual outcome.
The Endophthalmitis Vitrectomy Study specifically investigated the treatment of patients with endophthalmitis occurring within 6 weeks of cataract surgery. Patients were randomized to receive or not receive IV antibiotics and to undergo a vitrectomy/injection of intravitreal antibiotics or vitreous tap/injection of intravitreal antibiotics. The results of the study indicated the following:
1. There was no difference in final visual acuity/media clarity whether or not patients received systemic antibiotics.
2. Hand motions or better visual acuity on presentation did equally well with immediate vitreous biopsy or vitrectomy.
3. Eyes with light perception–only vision had much better visual outcome with immediate vitrectomy rather than vitreous biopsy.
37 D) Atherosclerosis
The causes of CRAO in children and young adults differ from those of the older population. In one study, one-third of the patients had a history of migraine. Other factors include trauma (especially in males), hypercoagulable states (oral contraceptives, pregnancy), cardiac emboli, collagen vascular disorders, and IV drug abuse. In the elderly population, atherosclerotic disease is much more common.
38 C) Rubeosis iridis
The incidence of rubeosis may be as high as 15% to 20% after CRAO. These patients may also develop neovascularization of the disk and retina.
39 A) Dalen–Fuchs nodules
Sickle cell retinopathy may have the following retinal findings: sunbursts (black chorioretinal scars from RPE hypertrophy and hyperplasia), salmon patch hemorrhages (subretinal blood), peripheral sea fan neovascularization, VH, and tractional retinal detachment. Angioid streaks may be associated with sickle cell disease. Dalen–Fuchs nodules are excrescences found at the level of Bruch membrane seen in sympathetic ophthalmia.
40 B) Rods
RP represents a collection of retinal degenerations with rod degeneration as the hallmark finding. A cone degeneration may occur secondarily.
41 D) The only effective treatment is enucleation of the traumatized eye.
After penetrating ocular trauma to one eye, bilateral granulomatous inflammation and panuveitis, known as sympathetic ophthalmia, may occur. The injured eye is known as the exciting eye, and the fellow eye is the sympathizing eye. Sympathetic ophthalmia may occur from weeks to many years after the injury, although it most often occurs within the first year. Treatment with steroids or immunosuppressive agents can be effective in suppressing the inflammation. In contrast to VKH disease, the choriocapillaris is uninvolved with the inflammation in sympathetic ophthalmia.
42 D) Nanophthalmos
POHS, angioid streaks, and pathologic myopia may lead to development of CNVMs. Nanophthalmos is associated with uveal effusions and serous retinal detachments.
43 B) Retinal break
In all patients who develop a macular pucker, the peripheral retina needs to be examined carefully to ensure that no retinal breaks exist. Retinal breaks may allow migration of RPE cells, which are thought to be able to transform into fibroblast-like cells, leading to epiretinal membrane formation.
44 D) 25%
In 15% to 25% of patients, a cilioretinal artery may be present to perfuse the macula. Pulsatile flow of blood with each heartbeat may be seen in these arteries. In the case of a CRAO, the cilioretinal artery may allow preservation of central acuity. Fluorescein angiography (Fig. 12-41) shows the extensive retinal arterial nonperfusion, except in the distribution of the cilioretinal artery in a patient with a CRAO.

FIGURE 12-41
45 D) Epiretinal membrane
Conditions that may have CME without leakage of fluorescein include Goldmann–Favre, RP, and nicotinic acid maculopathy. Epiretinal membranes may cause a CME that leaks from traction and distortion of paramacular capillaries.
46 A) Choroidal neovascularization (CNV)
A CNVM will cause subretinal hemorrhage or intraretinal hemorrhage. Preretinal hemorrhage would be very unusual. Sickle cell retinopathy, trauma (e.g., shaken baby syndrome), and macroaneurysms may cause hemorrhages at all levels of the retina.
47 D) Headaches and nausea
48 A) Optic nerve drusen
49 B) Gastrointestinal bleeding
50 A) CNV
Pictured in Figure 12-17 are angioid streaks in a patient with pseudoxanthoma elasticum. The radiating hyperfluorescent lines are window defects from a break in Bruch membrane. The predominant conditions associated with angioid streaks include Paget disease of bone, pseudoxanthoma elasticum, Ehlers–Danlos, and sickle cell disease.
Paget disease is a spectrum of findings, including osteoclastichyperactivity, especially at the base of the skull and in long bones. These patients are prone to pathologic fractures.
Sickle cell patients may have a number of retinal findings, including salmon patches, sea fan neovascularization, black sunbursts, and angioid streaks. They have a higher incidence of thrombotic episodes and may autoinfarct their spleens.
Ehlers–Danlos is a genetic disorder caused by a defect in collagen synthesis. The patients may have hyperextensible joints and lax skin. Ocular findings include dislocated lenses, retinal detachment, and blue sclera.
Pseudoxanthoma elasticum classically has the findings of angioid streaks, optic nerve head drusen, and a “peau-d’orange” appearance to the retina. These patients have cutaneous manifestations with the “plucked-chicken” appearance shown in Figure 12-42. They are prone to widespread vascular malformations. Abnormalities in the mucosal vasculature of the stomach and bowel can lead to recurrent hemorrhage.

FIGURE 12-42
51 D) Enucleation of the affected eye decreases the mortality rate.
Choroidal melanoma is a common intraocular tumor in adults that typically appears as an elevated, pigmented choroidal mass lesion. In a large retrospective study, the shields identified several factors that may help differentiate melanomas from choroidal nevi with the following pneumonic: “To Find Small Ocular Melanoma.” T = thickness >2 mm, F = fluid, S = symptoms, O = orange pigmentation (lipofuscin), M = margin-touching optic disk. The typical ultrasonographic finding is low-interal reflectivity given high vascularity. Enucleation was not associated with an improved 5-year mortality rate in the COMS study. Extraocular involvement can be hematogenous, with the liver being the most common site of distant metastasis, of direct extension into the orbit.
52 C) Maroteaux–Lamy
RPE degenerations have been identified in patients with Hunter, Hurler, Sanfilippo, and Scheie mucopolysaccharidoses. Maroteaux–Lamy syndrome is not usually associated with RPE degeneration.
53 D) Chloroquine
Retinal crystals may be seen in patients using tamoxifen, canthaxanthine, or methoxyflurane. Retinal crystals can also be seen in patients who have talc retinopathy. IV injection of talc crystals results in their distribution via the retinal circulation. Chloroquine or hydroxychloroquine can result in a bull’s-eye maculopathy as a result of disturbance of the RPE, but crystals are not present.
54 B) Nonperfusion on fluoresceinangiogram
Stargardt disease is an inherited retinal disorder that leads to vision loss during childhood or early adulthood. Yellowish flecks can be seen in the macula and peripheral retina. On fluorescein angiography, the choroid appears dark or “silent” due to blockage of choroidal fluorescence by excessive lipofuscin in the RPE. RPE atrophy in the macula can contribute to vision loss.
55 D) Vitrectomy and silicone oil tamponade
Rhegmatogenous detachments occur in up to 25% of patients with CMV retinitis. They are associated with a diffusely necrotic peripheral retina with numerous small retinal holes. These detachments cannot be repaired by conventional scleral buckling surgery, and they require pars plana vitrectomy with internal silicone oil tamponade and endolaser.
56 B) Myopia
Although exudative retinal detachments may occur in CMV retinitis, it is very uncommon. Myopia is not associated with exudative retinal detachments.
57 D) Irreversibly flat ERG
Intraocular copper foreign bodies may result in two distinct disease processes. One is a mild form called chalcosis. The other is a more severe suppurative form of endophthalmitis. The severity of intraocular inflammation is directly proportional to the concentration of copper within the foreign body. Chalcosis occurs in copper amalgams that contain significant amounts of nickel or other metals. Chalcosis is characterized by mild intraocular inflammation, development of a sunflower cataract, and Kayser–Fleischer rings. Characteristically, early removal of the intraocular foreign body in chalcosis can improve the amplitudes of the ERG, which have been suppressed from the presence of intraocular copper ions.
58 D) Anticoagulation with Coumadin
Various treatment modalities have been advocated for CRAOs, including methods to provide more oxygen to the ischemic retina (hyperbaric oxygen, carbogen), increasing perfusion of the retina (vasodilatory drugs, lowering IOP by anterior chamber paracentesis or administration of acetazolamide or mannitol), and fibrinolytic agents (intra-arterial t-PA). Animal studies have shown that irreversible damage occurs within 90 minutes of arterial obstruction. Warfarin requires several days to reach maximal effect and would not be helpful in an acute situation.
59 A) It occurs in eyes with abnormally short axial length.
Uveal effusion syndrome usually occurs in eyes with abnormally short axial length. These eyes often will have thickened sclera, which are thought to impede vortex venous outflow from the eye, resulting in recurrent choroidal effusions. Treatment is often unrewarding but involves the placement of partial thickness scleral windows near the vortex vein exit sites in at least three or four quadrants of the eye. Choroidal effusions or hemorrhage can occur during or after intraocular surgery and are thought to be caused by rapid changes in IOP–shearing choroidal perforating arteries. Hypertension and atherosclerosis are risk factors for choroidal effusions.
60 B) Observation
Traumatic macular holes usually result from preexisting commotio in the region of the macula. They are characterized by disruption and necrosis of retinal photoreceptors and subsequent loss of retinal tissue. Unlike idiopathic macular holes, which are caused by tangential traction on the macula where vitrectomy and gas–fluid exchange have successfully closed the hole, surgery is not, in general, the treatment for traumatic holes. There have been several reports of improvement in vision in traumatic holes with vitrectomy, gas–fluid exchange, and application of TGF-β.
61 A) Sand
Inert foreign bodies, such as glass, plastic, sand, stone, or ceramic, are well-tolerated in the eye. Wood incites a brisk inflammatory reaction and may harbor harmful microorganisms. Brass contains copper, which may lead to chalcosis and retinal degeneration. Iron is tolerated poorly within the eye. Intraocular iron causes siderosis, resulting in photoreceptor and RPE degeneration.
62 C) Disruption of photoreceptor elements and damage to photoreceptor cells
Commotio represents an actual disruption or destruction of retinal photoreceptor elements and photoreceptor cells in the outer layers of the retina. It does not represent retinal edema.
63 C) 3 > 4 > 2 > 5 > 1
The most common traumatic retinal tear is an inferotemporal retinal dialysis. The vast majority of retinal dialyses occur in this quadrant. After trauma, the most common retinal tear is a superonasal dialysis, followed by giant tears, flap tears, and tears around lattice. These statistics are true only for blunt ocular injury.
64 B) Has a good visual prognosis with complete healing of retinal injuries
Shaken baby syndrome may be associated with retinal hemorrhages and cotton-wool spots that have the appearance of a CRVO or Purtscher retinopathy. This retinal injury often has a poor prognosis because of associated macular scarring, VH, and retinal detachment. Associated neurologic damage is common.
65 C) Both A and B
The original description by Terson consisted of both retinal and VHs in patients who have subarachnoid and subdural hemorrhages. About 20% of patients with spontaneous or traumatic subarachnoid hemorrhages will present with intraocular hemorrhages.
66 D) Disseminated intravascular coagulation
Purtscher retinopathy does not occur from disseminated intravascular coagulation. Disseminated intravascular coagulation can result in fibrinoid necrosis of the choriocapillaris, serous retinal detachments, and multiple areas of RPE changes. However, numerous cotton-wool spots, subinternal limiting membrane hemorrhages, and retinal hemorrhages are uncommon in this condition.
67 B) Increased risk of rhegmatogenous retinal detachment
Coats disease is characterized by telangiectatic changes in the retinal vasculature. The condition is commonly unilateral and shows a male predominance. Microvascular changes can leak and lead to exudative retinal detachment, which may be treated with laser photocoagulation.
68 A) Is initially associated with a clear lens or minimal opacity that may later become densely cataractous
PFV, sometimes referred to as persistent hyperplastic fetal vasculature is a developmental malformation of the eye that results from failure of regression of the primary hyaloid and other intraocular vessels. It is associated with microphthalmia. Although typically unilateral, it may be bilateral in up to 10% of cases. In such cases, the lack of a history of low birth weight may help differentiate bilateral PFV may aid in differentiating it from retinopathy of prematurity, which is strongly associated with low birth weight. Some cases of PHPV may simply be observed or treated with lensectomy.
69 A) Granulomatous keratic precipitates are found in both eyes.
Granulomatous keratic precipitates are a characteristic presentation of sympathetic ophthalmia. Sympathetic ophthalmia occurs in less than 0.1% of cases of penetrating ocular injury. It is even less common after intraocular surgery. It is thought to result from immune sensitization to melanin or melanin-associated proteins in the uveal tissues, which results in bilateral granulomatous panuveitis. Once the inflammation has started in the contralateral eye, the role of enucleation of the inciting eye in reducing inflammation is very controversial and may not be beneficial.
70 C) Topical and systemic corticosteroids
Sympathetic ophthalmia often responds to corticosteroids with quieting of inflammation and improvement in vision. If steroids are not tolerated or are ineffective, immunosuppressive drugs may be necessary. Vitrectomy or injection of intravitreal antibiotics may be indicated for cases of endophthalmitis but not for sympathetic ophthalmia.
71 C) Measles
White-centered hemorrhages can be found in conditions with septic emboli (endocarditis, Candida bacteremia), leukemia, and collagen vascular diseases. Measles causes white-centered hemorrhages (Koplik spots) on the buccal mucosa, but retinal hemorrhages are not found.
72 C) Viral prodrome
PIC is an entity that is slightly more common in myopic women in the third and fourth decades of life. It may be associated with recurrent CNVMs. It is not, however, associated with a viral prodrome as is APMPPE.
73 C) Viral prodrome
APMPPE is a condition that is seen in the second to fourth decades of life. It is often preceded by a viral illness. Males and females are equally affected. Visual loss can be severe at the onset but, over the course of 4 to 6 weeks, visual acuity improves in most patients. White placoid lesions at the level of the RPE and choriocapillaris are characteristic of the acute phases of this disease. Vitritis is minimal or absent. These lesions then subsequently fade over 4 weeks and result in RPE disruption.
74 B) Late hyperfluorescence of lesions
Fluorescein angiography of APMPPE is characterized by early hypofluorescence of lesions, followed by late hyperfluorescence of the entire lesion. Rarely, perivascular staining may be seen. Because of pigmentary disturbances that occur in the healed cases, CNVMs can develop, although it is extremely rare.
75 A) Early hypofluorescence of white dots
Fluorescein angiography in MEWDS is characterized by early punctuate hyperfluorescence, often in a wreath-like configuration, followed by late staining of the same punctate areas of hyperfluorescence. These areas of hyperfluorescence correspond to the white spots seen clinically. Late disk staining is also a common feature.
76 C) CNV
CNV is by far the most common macular complication of multifocal choroiditis. This is the major cause of vision loss in most patients with multifocal choroiditis.
77 C) Adult onset foveomacularvitelliform dystrophy
The EOG shows a diminished light-peak-to-dark-trough ratio, characteristically below 1.7, in patients who have Best disease and in patients who are carriers of Best disease. Adult onset foveomacular vitelliform dystrophy is not associated with an abnormal EOG. Patients with this particular disorder may present with a ringlike area of RPE clumping in the early phases. Over the course of many years, this area will develop into a yellowish lesion that is typically one-half disk diameter in size or slightly smaller, occupying the central fovea. These lesions are much smaller than those seen in Best disease. This disorder is associated more commonly with CNV than is Best disease.
78 C) More effective than fluorescein angiography for imaging choroidal circulation
ICG absorbs from 790 to 805 nm, and has an emission spectrum from 770 to 880 nm, peaking at 835 nm. Activity in the near-infrared spectrum allows better visualization through media hemorrhage, serous detachment and lipid exudation. Under physiologic conditions, it remains 98% protein-bound. Since less dye escapes the choroidal vessels, and less fluorescence is absorbed by overlying retinal pigment, ICG angiography highlights choroidal circulation more than fluorescein anigography.
79 A) Nerve fiber layer
80 A) Nerve fiber layer
81 C) Outer plexiform layer
Retinoschisis is an actual splitting of the cellular layers of the retina. JXLR typically is associated with schisis at the level of the nerve fiber layer. The earliest macular changes may include parafoveal spoke-wheel type appearance to these dehisciences of the nerve fiber layer. As the disorder progresses, bullous schisis cavities develop with eventual obliteration of this very thin inner layer of tissue. Retinal vessels subsequently are the only things that may remain within this inner layer of tissue. These blood vessels have a propensity for bleeding and producing VHs. Once they become sclerotic, they may have the appearance of “vitreous veils.” Holes in the outer layers of the retina may subsequently predispose patients with retinoschisis to the development of rhegmatogenous retinal detachment.
Reticular retinoschisis is characterized by an involutional splitting of the retina in the nerve fiber layer. This change may be seen as a spectrum of change that begins as microcystoid peripheral retinal degeneration. Reticular retinoschisis may also be seen with the more common involutional retinoschisis that is associated with splitting at the outer plexiform layer. Typical involutional retinoschisis is located most commonly in the inferotemporal quadrants of the peripheral retina. It often can be mistaken for a rhegmatogenous retinal detachment. Rhegmatogenous retinal detachments can occur in the presence of outer retinal holes.
82 B) Thioridazine-induced retinopathy
Thioridazine may induce significant RPE atrophy alternating with areas of clumping but does not characteristically produce a bull’s eye maculopathy.
83 C) CME
The hallmark of JXLR is bilateral, splitting of the nerve fiber layer in the central macula, but peripheral retinoschisis can also be found in many cases. VH can further compromise vision in these individuals. The typical ERG finding in JXLR is a normal a wave with a diminished or “negative” b wave.
84 A) Mizuo–Nakamura phenomenon
Oguchi disease is an X-linked recessive form of congenital stationary night blindness. It is associated with the Mizuo–Nakamura phenomenon, which is the appearance of a golden brown fundus in the light-adapted state with a normalization of the color of the fundus on dark adaptation.
85 A) Ornithine transcarbamylase deficiency
Gyrate atrophy is a metabolic disorder that is seen mainly in Scandinavian Laplanders. It is associated with a deficiency in the ornithine aminotransferase enzyme, critical in the urea cycle. This results in an accumulation of serum ornithine. The end result is that of an RPE degeneration that begins in the periphery and is characterized by scalloped areas of RPE loss with eventual loss of choriocapillaris and medium-sized choroidal vessels. Recent research has suggested that the ornithine aminotransferase gene is located on chromosome 10; therefore, abnormalities on chromosome 10 may result in gyrate atrophy.
86 B) ERG amplitudes are reduced in the carriers of choroideremia.
ERG amplitudes in carriers of choroideremia are typically normal, unlike carriers of juvenile X-linked RP. However, female carriers of choroideremia do show midperipheral pigmentary changes and choroidal atrophy.
87 C) Optic disk hyperemia
RP is an inherited retinal degeneration that can show autosomal dominant, autosomal recessive, and X-linked recessive patterns of inheritance. Typical findings include increased pigmentation in the peripheral retina (“bony spicules”), vascular attenuation, optic disk pallor, CME, and PSC.
88 A) Oculocutaneous albinism usually has autosomal dominant inheritance.
Oculocutaneous albinism is inherited typically in an autosomal recessive manner. Other ocular manifestations include iris transillumination defects and nystagmus secondary to poor vision from foveal hypoplasia.
89 B) Reticuloendothelial dysfunction
90 A) Platelet dysfunction
Hermansky–Pudlak syndrome and Chediak–Higashi syndrome are both potentially lethal autosomal recessive diseases that present with albinism. Hermansky–Pudlak syndrome has abnormal platelets that may lead to a bleeding diathesis. In Chediak–Higashi syndrome, a disorder in microtubule formation results in leukocytes that cannot release enzymes from lysosomes. This disorder increases the risk of recurrent pyogenic infections.
91 B) 67%
The presence of VH in association with a posterior vitreous detachment is highly suggestive of the presence of a retinal tear. Repeat examination is advised in the first 2 weeks after onset of posterior vitreous detachment and VH if a retinal tear is not found initially. Ultrasound evaluation may also be useful.
92 B) Retinal detachment in the fellow eye
Although myopia, lattice degeneration, and a family history of retinal detachments are important factors and are associated with higher-than-normal risk of retinal detachment, retinal detachment in the fellow eye increases the chance of retinal detachment to approximately 10% to 15%. Myopia, especially moderate myopia, is the next highest risk factor (7%–8%), followed by family history and lattice degeneration.
93 A) 50%
Patients with a giant retinal tear in one eye are at very high risk of retinal detachment in the fellow eye. However, this risk is not 100%.
94 A) The causative organism is a bacterium.
The causative agent of toxoplasma retinitis is the protozoa Toxoplasma gondii. It often presents with a panuveitis in addition to the retinitis. A focal area of active retinitis often appears yellowish or whitish with indistinct margins, often adjacent to a hyperpigmented scar representing an area of previous retinitis. The panuveitis often obscures a sharp view of the retinitis, which may give a “headlight in the fog” appearance. Although episodes are often self-limited, antibiotic treatment, classically with pyrimethamine, sulfadiazine and folic acid (“triple therapy”) and oral prednisone may be useful in limiting the course and extent of damage from the disease, especially if the lesion is near the macula. Involvement of the CNS can occur, especially in the setting of immunosuppression.
95 D) Attachment of the macula
The most important factor that determines visual outcome in the presence of a retinal detachment is whether the macula is attached or detached at the time of presentation. The duration of macular detachment may also play a role in determining final visual outcome, especially if the macula has been detached for less than 24 hours. VH and pigment cells in the vitreous increase the risk of proliferative vitreoretinopathy, but these are not factors in determining visual outcome.
96 D) Proliferative vitreoretinopathy
Proliferative vitreoretinopathy is the most common reason for failure of scleral buckling surgery. A 5% to 10% chance of failure of primary scleral buckling exists in cases of rhegmatogenous retinal detachment.
97 D) 6 o’clock
Figure 12-22 shows an inferior retinal detachment with an equal level of subretinal fluid progression nasally and temporally, suggesting that a break is probably present at approximately 6 o’clock.
98 C) 3 o’clock
Figure 12-24 shows an inferior detachment. However, the fluid level is higher on the nasal side than on the temporal side. In this situation, the most likely position for the break is on the side where the subretinal fluid level is higher.
99 A) 12 o’clock
In Figure 12-24, the break may be located anywhere between the 10- and 2 o’clock meridians, but it is most likely located between 10- and 12 o’clock.
100 B) 9 o’clock
In Figure 12-25, the fluid level is higher on the temporal aspect (9 o’clock), and the break is most likely present temporal. The fluid has not reached the 12 o’clock meridian. The area between 3 o’clock and 12 o’clock should be examined for breaks as well.
101 C) Should be treated with scleral buckle and vitrectomy with internal drainage of the subretinal fluid
Exudative retinal detachments are not treated with scleral buckle, vitrectomy, or scleral drainage of subretinal fluid. The etiology of such detachments must be determined. Exudative retinal detachments typically are characterized by shifting subretinal fluid, and they can be quite bullous. Many intraocular tumors may be associated with serous retinal detachments, including choroidal melanomas and hemangiomas.
102 D) JXLR
All of the conditions listed in this question cause traction retinal detachments except JXLR, which typically is associated with rhegmatogenous retinal detachments and VHs.
103 D) Systemic hypercalcemia
Asteroid hyalosis is a common, unilateral finding that represents calcium soaps suspended in the vitreous gel. Patients are remarkably asymptomatic and do not often complain of decreased vision or floaters. No association with any systemic abnormalities exists.
104 A) Previous blunt trauma with hyphema
Synchysis scintillans can be seen in patients after resolution of a VH. Refractile, yellow, cholesterol crystals usually float freely in the liquefied vitreous and will settle inferiorly with time. A systemic hyperlipidemic state is not necessary.
105 B) Perfluoropropane (C3F8)
Intraocular gases can provide tamponade of retinal breaks. The longest-lasting gas is C3F8, in which over 50% of the gas will still be present in 3 weeks. The duration is less with C2F6, SF6, and shortest with air.
106 C) 100% SF6
SF6 has the highest expansile rate for any intraocular gas. It can cause dramatic increases in IOP in the early postoperative period.
107 C) Less than SF6 against retina
Surface tension of silicone oil is significantly less than the surface tension of all gases, including air.
108 B) Less than water
Silicone oil is buoyant when placed in a fluid-filled eye. The specific gravity of gases, such as perfluorooctane, is much less than that of water or any liquid.
109 C) Erythrocyte sedimentation rate (ESR)
110 A) Decreased b-wave amplitude
111 A) Systemic corticosteroids and temporal artery biopsy
Figure 12-26 is an arteriovenous phase of fluorescein angiogram that reveals choroidal nonperfusion. This is most consistent with an ischemic event that involves the short posterior ciliary arteries. This has resulted in not only an anterior but also a posterior ischemic optic neuropathy in the left eye. This is a characteristic presentation of patients with temporal arteritis. ESR often is elevated dramatically. Immediate treatment with systemic corticosteroids and temporal artery biopsy are indicated to confirm the diagnosis.
The ERG measures the mass response of the retina to a light stimulus. The a wave measures the depolarization of the photoreceptors. The b wave records the function of the inner retinal elements (Müller and bipolar cells). This wave would be affected most profoundly by a CRAO. The implicit time is the time between the trough of the a wave and the peak of the b wave. Increased implicit times may be found in various hereditary conditions. The flicker stimulus is used to selectively measure the cone response because rods are unable to cycle quickly enough.
112 B) Unilateral shimmering photopsias
113 A) More common in women
114 B) Enlarged blind spot on visual field testing
The patient in Figure 12-27 has characteristic MEWDS. This disorder typically occurs in females in the third and fourth decades of life. It is often associated with symptoms of shimmering photopsias and paracentral scotomas. Some patients may have a flu-like illness preceding their symptoms. These scotomas often correspond to an enlarged physiologic blind spot on visual field testing. The disorder is typically self-limited, with resolution occurring between 3 and 10 weeks after onset. Usually, no treatment is necessary. However, patients may have decreased vision despite resolution of the syndrome as a result of pigmentary changes in the fovea that have a characteristic granular appearance. In addition, 10% to 15% of patients may have recurrent episodes in the same eye or in the fellow eye.
Mild to moderate myopia has been found in many patients with PIC.
115 D) Autosomal recessive inheritance
116 C) Accumulation of lipofuscin granules in the RPE
117 D) ERG amplitudes are often normal.
The fluorescein angiogram in Figure 12-28 reveals the characteristic silent choroid appearance of this patient with Stargardt disease. This disorder is inherited in an autosomal recessive fashion. Patients are often asymptomatic. Vision may be good on presentation. Clinical examination may reveal yellow flecks in the posterior pole and pigmentary changes in the macula. On fluorescein angiography, these pigmentary changes show up as window defects, and there is blockage of underlying choroidal fluorescence and the appearance of the classic dark or silent choroid. Yellow flecks in the retina are not hyperfluorescent. These flecks are caused by lipofuscin granules that have accumulated in the RPE, blocking underlying choroidal fluorescence. Electrophysiologic testing in these patients often is not helpful. Examination of family members may be useful.
118 C) Cone dystrophy
119 C) Chloroquine
120 A) Abnormal photopic ERG
The fluorescein angiogram in Figure 12-29 is characteristic of a bull’s eye maculopathy. It may be seen in cone dystrophy, chloroquine toxicity, Batten disease, and rarely in RP. Other toxic retinal pigment epitheliopathies may result in an appearance similar to a bull’s eye maculopathy, but true bull’s eye maculopathy is rare. In cases of cone dystrophy, electrophysiologic findings suggest a diminished cone ERG response.
121 B) Early arterial
122 A) Choroidal
123 B) Early arterial
124 A) Choroidal
The timing of the filling of a lesion with fluorescein depends on its source of blood. Choroidal lesions (e.g., malignant melanomas, cavernous hemangiomas) will fill with the choroidal phase early in the angiogram. The cilioretinal artery also fills with the choroid because it is a branch of the posterior ciliary artery rather than the ophthalmic artery. The capillary hemangioma and NVD would fill with the retinal circulation.
125 C) Photoreceptors, bipolar cells, RPE
Ganglion cells do not contribute to the ERG response. The ERG may be normal in the presence of total disk cupping. The negative a wave (late receptor potential) originates in the photoreceptors. The positive b wave originates in the bipolar cell layer, probably in response to increased potassium concentration in the extracellular space of the bipolar cells. The positive c wave appears to originate from the RPE.
126 D) It has a poor visual prognosis
Visual prognosis is good. Most patients retain reading vision in at least one eye throughout life. The progression of visual loss is slow and occurs for the most part beyond the age of 40 years.
127 A) 12%
A simplified severity scale was developed from the AREDS to estimate likelihood of progression to CNV after 5 years. The scoring system assigns to each eye one point for the presence of large drusen, one point for the presence of any pigment abnormality, and two points for advanced ARMD. Risk factors are summed across both eyes, yielding a five-point scale (0–4) on which the approximate 5-year risk of developing advanced ARMD in at least one eye increases:
• 0 point, 0.5%
• 1 point, 3%
• 2 points, 12%
• 3 points, 25%
• 4 points, 50%
In this case, the patient has large drusen in each eye, so she has 2 points, and has a 12% chance of developing choroidal neovasculization in 5 years.
128 A) Age-Related Eye Disease Study (AREDS) formulation
The AREDS was a randomized, placebo-controlled trial that showed that a combination of antioxidants and zincs ([vitamin C [500 mg], vitamin E [400 IU], vitamin A [β-carotene, 15 mg] zinc [80 mg plus 2 mg copper]) reduced the progression to advanced ARMD by 25% in patients with intermediate ARMD (defined as extensive [>6] intermediate drusen [>64 µm in size] or with large drusen (>125 µm; width of a large vein at disc margin). Patients with early ARMD had no benefit. The use of high-dose β-carotene (vitamin A) was cautioned in current or former smokers due the possible increased risk of lung cancer. The AREDS 2 study showed that omega-3 fatty acids had no protective effect. A multivitamin would not be appropriate here.
129 C) Vitamin A
The use of high-dose β-carotene (vitamin A) was cautioned in current or former smokers due the possible increased risk of lung cancer.
130 D) All of the above
Figure 12-31 demonstrates many classic features of PDR, showing extensive leakage from NVD and NVE, hypofluorescence from a blocking defect caused by VH, and diffuse peripheral capillary nonperfusion.
131 A) Pars plana vitrectomy
This patient has PDR with high-risk characteristics, and the Diabetic Retinopathy Study has shown that PRP decreases the risk of severe visual loss by 50%. Given the presence of VH, there may not be an adequate view for PRP, and close observation within 1 month would also be appropriate to allow the VH to settle. There is growing clinical and anecdotal evidence to suggest that intravitreal anti-VEGF agents may also have efficacy in treating active PDR. Anti-VEGF agents may not only cause regression of neovascularization, but also help with the macular edema component of the disease. Indications for pars plana vitrectomy include traction retinal detachment, nonclearing VH, and/or recurrent VH. Most retina specialists prefer to delay PPV until adequate PRP has been performed.
High-risk PDR was also defined as three or more of the following high-risk characteristics (HRC’s):
1. Presence of vitreous hemorrhage or pre-retinal hemorrhage
2. Presence of any active neovascularization
3. Location of neovascularization on or within one disc diameter of the optic disc
4. NVD > 1/3 disc area or NVE > ½ disc area
Eyes with high-risk PDR had significantly greater risk of severe visual loss and demonstrated the greatest benefit from PDR.
No clear benefit was demonstrated for PRP in eyes with severe NPDR or in eyes with PDR without high-risk characteristics.
132 C) Figure 12-34
Retinal artery macroaneurysms are not associated with CNVMs. They are abnormal outpouchings of the retinal vasculature, usually seen in elderly hypertensive females. The other three conditions mentioned, idiopathic central serous chorioretinopathy, myopic macular degeneration, and exudative ARMD, may all be associated with CNVMs.
133 C) Carotid Doppler and cardiac echocardiography
Figure 12-36 shows a Hollenhorst plaque and inferotemporal branch retinal artery occlusion. A source of the emboli must be sought. The most common origin is either from the heart or from an atherosclerotic plaque in the carotid arteries, especially at the junction of the external and internal carotid arteries.
134 A) Figure 12-37
Figure 12-37 depicts a stage IV idiopathic macular hole. The diagnosis of a full-thickness macular hole can usually be made on clinical and biomicroscopic grounds alone. Treatment (vitrectomy surgery) depends on factors such as stage of the hole, visual acuity, and length of time that the hole has been present. There is no place for laser photocoagulation in this condition.
135 B) Systemic hypertension
Retinal artery macroaneurysm is encountered most commonly in elderly hypertensive females.
136 A) Stage I
Stage I corresponds to an impending macular hole. In a randomized control trial, vitrectomy has been shown not to be indicated for impending macular holes because the natural history results in a better outcome than in patients undergoing vitrectomy surgery. Vitrectomy surgery results in improved visual acuity in patients with stage II, III, and IV macular holes.
137 D) Stage IV
Stage IV macular hole is defined as a full-thickness hole in the presence of posterior vitreous separation. In stage I macular holes, there is foveal separation but no actual retinal break. In stage-II and -III macular holes, by definition, the posterior hyaloid is still attached.
138 B) Figure 12-36
There is no role for laser therapy in managing branch retinal artery occlusions. The risk of retinal neovascularization in branch retinal artery occlusion is almost nonexistent. Diabetic macular edema, retinal artery macroaneurysms, and exudative ARMD may all be treated with laser photocoagulation.
139 D) Figure 12-33
Figure 12-33 shows a case of exudative AMD. There is a large subretinal hemorrhage with a pigment epithelial detachment. If the fluorescein angiogram shows evidence of an occult CNVM, ICG demonstrates a treatable lesion in up to 40% of ARMD patients with a fibrovascular pigment epithelial detachment.
140 C) Proliferative vitreoretinopathy
Proliferative vitreoretinopathy results in cellular proliferation on the surface of the retina and not an exudative maculopathy with edema, as can be seen in the other three conditions.
141 B) Extramaculartractional retinal detachment
If a tractional retinal detachment is present without a rhegmatogenous component, and if the macula is still attached, the patient can be monitored closely. If the macula detaches, or if there is progression of the detachment and the macula is threatened, vitrectomy surgery should be considered.
142 C) Choroidal neovascular membrane (CNVM)
CNVM is rarely seen accompanying a macular pucker. Its presence is not, however, an indication for surgery.
143 C) Kearns–Sayre syndrome
Jansen and Wagner syndromes are characterized by vitreous liquefaction without associated systemic manifestations. Stickler syndrome is related to these with the addition of a flat facies and Pierre Robin sequence abnormalities. Kearns–Sayre syndrome is associated with retinal pigmentary changes, CPEO, and cardiac abnormalities.
144 C) Male gender
Increased age, smoking, female gender, and a diet low in antioxidants and lutein have been shown to be risk factors for CNV in ARMD. Male gender is not a risk factor.
145 C) POHS
ARMD is usually seen in patients above the age of 50 years. They have drusen and RPE changes in the macula.
Toxoplasmosis is usually accompanied by anterior chamber, vitreous cell, and focal retinitis lesions often occurring at the edge of a previous scar. Multifocal choroiditis and panuveitis may present like POHS but have the following differences: (1) vitreous inflammation, (2) inactive lesions are generally smaller than those in POHS, (3) anterior uveitis occurs in 50% of cases, (4) most patients come from areas nonendemic for histoplasmosis and have a negative histoplasminskin test, (5) about 50% demonstrate a subnormal ERG, (6) female gender predilection, and (7) more frequent in children.
146 C) Chorioretinal scar
Although a CNVM may arise from a chorioretinal scar, the scar itself is not a clinical sign of CNVM as are the other findings.
147 C) Subfoveal
According to the results of the Macular Photocoagulation Study, eyes with POHS with well-defined extrafoveal or juxtafoveal CNVMs that were untreated were at a much greater risk of a six-line decrease in visual acuity from the 1-year through the 5-year examination than were eyes treated with laser photocoagulation.
148 D) Operculated holes secondary to vitreous traction
Patients with lattice retinal degeneration are at higher risk for retinal detachments because of the strong attachments of the vitreous to the edges of these lesions. Traction causes horseshoe tears. Holes found in lattice are more atrophic with no associated tractional component.
149 A) Louis–Bar
Wyburn–Mason has arteriovenous malformations, von Hippel–Lindau has retinal hemangioblastomas, and Bourneville syndrome (tuberous sclerosis) may have astrocytic hamartomas. Louis–Bar, or ataxia–telangiectasia, does not have characteristic retinal changes.
150 D) Subretinal scarring
Subretinal scarring is an uncommon complication of RP. Pigment disturbances, which may be perivascular and appear as bone spiculing in the midperiphery, are common. CME and epiretinal membrane formation also commonly occur. Large areas of macular atrophy have also been described. Optic disk drusen may also occur in patients with RP.

